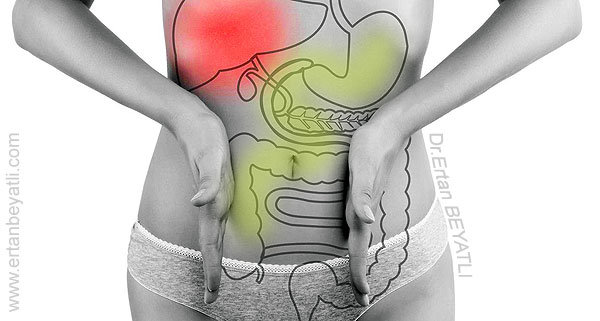
Postkolesistektomi Sendromu (PKS) terimi, Safra kesesi ameliyatı (kolesistektomi) sonrası semptomların varlığını tanımlar. Bu semptomlar, safra kesesi patolojisinin neden olduğu düşünülen semptomların devam etmesini veya safra kesesine atfedilen yeni semptomların gelişimini gösterebilir. PKS ayrıca safra kesesinin çıkarılmasından kaynaklanan semptomların gelişimini de (örn., Gastrit ve diyare) içerir.
İlgili makale: Safra Kesesi Ameliyatı için doğru karar nasıl verilir?
Genel olarak PKS bir ön tanıdır ve yeterli bir çalışma sonucunda tanımlanan hastalıkla ilişkili olarak yeniden adlandırılması gerekir. Safra kesesinin rezervuar fonksiyonunun kaybına bağlı olarak safra akışındaki değişikliklerden kaynaklanmaktadır. İki tür problem ortaya çıkabilir.
- Birincisi, üst sindirim (gastrointestinal GI yolu) sistemi içinde artan safra akışı, örn. özofajit ve gastrit.
- İkincisi, diyare ve karın ağrısı gibi alt sindirim (GI yolu) sistemi ile ilgilidir. Bu yazı genel olarak PKS’nin genel konularına değinmektedir.
PKS hastaların yaklaşık %10-15‘ini etkilediği bildiriliyor.
PKS’nin şüpheli semptomlarını ortaya çıkarmak için, sıklıkla öngörülen ameliyat sonrası problemlerin ortaya çıkmasına yönelik spesifik bir araştırmayla, hastalar ve hekimleri arasında etkili iletişim gerektirir. Tedavi, yapılan özel teşhise göre yapılmalı ve farmakolojik veya cerrahi yaklaşımları içerebilir.
Patofizyoloji ve Etiyoloji
Hafif sindirim sorunlarında bile hastalarda PKS sebep olarak düşünülmektedir. Safra kesesinin rezervuar fonksiyonunun ortadan kaldırılması safra akışını ve safranın enterohepatik dolaşımını değiştirir. PKS’nin patofizyolojisi, safra akışındaki değişikliklerle ilişkilidir ve henüz tam olarak anlaşılamamıştır. Anatomik Konuma Göre Postkolesistektomi Sendromunun Etiyolojisi şöyledir:
Safra kesesi kalıntısı ve sistik kanal
- Kalıntı (rezidü) veya kısmi safra kesesi (Parsiyel Kolesistektomi)
- Stump Kolelitiyazis (safra kanalının uzun bırakılması sonucu oluşan taşlar)
- Nörom (sinir hücrelerinin tümörü)
Karaciğer
- Karaciğerin yağ infiltrasyonu (hepatosteatöz)
- Hepatit
- Hidrohepatosis (koledokun tıkanma sonucu)
- Siroz
- Kronik idiyopatik sarılık
- Gilbert hastalığı
- Dubin-Johnson sendromu
- Hepatolitiazis (karaciğerde taş oluşması)
- Sklerozan kolanjit (safra yollatı iltihabı)
- Kist
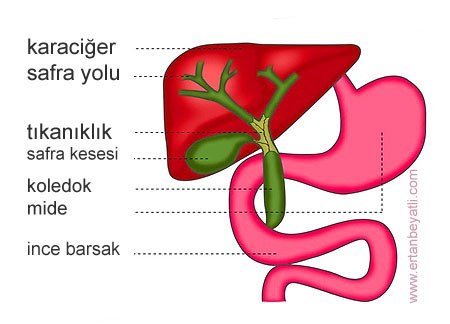
Biliyer kanal (Safra Yolları)
- Kolanjit
- Adezyonları (yapışıklıklar)
- Darlıklar (striktür)
- Travma
- Kist
- Malignite ve kolanjiyokarsinoma
- Tıkanıklık (obstrüksiyon)
- koledokolitiyazis (ana safra yollarında taş oluşması)
- Obstrüksiyonsuz dilatasyon (tıkanıksız genişleme)
- Hipertansiyon veya spesifik olmayan genişleme
- Diskinezisi
- Fistül
Periampuller (ampulla of Vater)
- Oddi sfinkterinde diskinezi, spazm veya hipertrofi
- Oddi sfinkterinde striktür
- Papilom (siğil)
- Kanser
Pankreas
- Pankreatit
- Pankreas taşı
- Pankreas kanseri
- Pankreatik kistler
- Benign tümörler
Yemek borusu (özofagus)
- Aerofaji (fazla hava yutma ve gürültülü geğirti)
- Diyafragma hernisi
- Hiatal herni
- Akalazya (alt yemek borusu spazmı vedarlığı)
Mide
- Safra gastriti (Alkalen Reflü Gastrit)
- Peptik ülser hastalığı
- Mide kanseri
İnce ve Kalın bağırsak
- Adezyonlar
- Duodenal divertikül
- Ameliyat sonrası kesi yerinde oluşan fıtık (insizyonel henri)
- Kabızlık (konstipasyon)
- İshal (diyare)
- İrritabl bağırsak hastalığı (İBS)
Damar
- Bağırsak anjinası (barsak krizi)
- Koroner angina (kalp krizi, anjina pektoris)
Sinir
- Nörom
- Interkostal nevralji (ameliyat bölgesinde kaburga kemiği ağrısı)
- Omurilik sinir lezyonları
- Sempatik dengesizlik
- Nevroz
- Ruhsal gerginlik veya endişe
Kemik
- Artrit
Diğer
- Adrenal kanser
- tirotoksikoz
- Safra taşıları ve cerrahi klipsleri de içeren yabancı cisimler
Bazı çalışmalarda ameliyat sonrası dönemde gastritin daha sık olduğu tespit edilmiştir (Abu Farsakh ve arkadaşları %30’a karşı %50). Kolesistektomi sonrası açlık gastrik safra asit konsantrasyonunun arttığını ve PKS’li hastalarda artışın daha fazla olduğu gösterildi. Yapılan ikinci cerrahi girişimlerde bile hastaların %8’inde tanı konulmamaktadır. Yapılan çalışmalarda safra kesesi ameliyatı geçiren hastaların %14’ünde PKS riskinin var olduğu gözlemlenmiştir. PKS riski ameliyat öncesi (preoperatif) bulgularla ilişkili olmadığı da tespit edilmiştir.

Safra Kesesi ameliyatı için bazı Önemli hususlar:
- Acil şartlarda yapılan ameliyatlarda PKS gelişime riskli daha yüksektir.
- Safra kesesinde taş varsa, hastaların %10-25’inde; taş yoksa, hastaların %29’unda PKS gelişebilir.
- Ameliyat öncesi şikayet süresi 1 yıldan az ise, hastaların %15.4’ünde; 1-5 yıl ise, %21; 6-10 yıl ise, %31’inde ve 10 yıldan fazla ise ,%34’ünde PKS gelişebilir.
- Amelyat esnasında Safra yolları açılırsa (Koledokotomi), hastaların %23’ünde; Koledokotomi yapılmazsa, %19’unda PKS gelişebilir.
- Safra Kesesi ameliyatının yararları ve zararları
Yaş ve cinsiyete bağlı demografik bilgiler
Kadınlarda PKS oranı %28 iken erkeklerde %15‘dir. Çalışmalara göre yaş farkı şöyledir:
- 20-29 yaş arası olanlarda %43
- 30-39 yaş arası olanlarda %27
- 40-49 yaş arası olanlarda %21
- 50-59 yaş arasındaki olanlarda %26
- 60-69 yaş arası olanlarda %31
- 70 yaşın üzerindeki hastalar PKS gelişmedi
- Dr.Ertan BEYATLI
Prognoz
Sonuç ve prognoz, hastanın çeşitliliğine, karşılaşılan koşula ve gerçekleştirilebilecek ameliyatlara göre değişir. Moody, hastalarının %75‘inde uzun süreli takiplerde ağrının iyi bir şekilde azaltıldığını gösterdi. Kısa süreli komplikasyonlar sık görülür (%5-40). Hiperamilasemi en sık görülen komplikasyondur ancak genellikle ameliyat sonrası 10. günde düzelir. Olguların %5’inde pankreatit, %1‘inde ise ölüm görülmesi beklenir.
Tarihçe
Postkolekistektomi Sendromlu (PKS) hastalarda çok çeşitli semptomlar görülebilir. Semptomlar bazen safra kesesi ile ilişkili olarak düşünülür. Freud, hastaların %93’ünde kolik, %76’sı ağrı, %24’ünde sarılık ve %38’inde ateş buldu. Yazarın hasta grubundaki PKS oranı %14’tür. Hastaların %71’inde ağrı, %36’sında ishal veya bulantı, %14’ünde şişkinlik veya gaz bulunur. PKS’nin nedeni, hastaların %95’inde tanımlanabilir. Dr.Ertan BEYATLI
Fiziksel Muayene
PKS’nin çalışması değişiktir. Belirtilerin spesifik bir nedenini saptamaya ve ciddi post-kolesistektomi komplikasyonlarını dışlama girişiminde hastanın kapsamlı bir çalışması yapılmalıdır. Yeniden incelemede cerrahi müdahale son çare olarak düşünülmelidir. Hasta muayenesi kapsamlı bir geçmişi ve dikkatli bir fizik muayene ile başlar. Ameliyat öncesi muayene ve teşhis, cerrahi bulgular ve patolojik muayene ve postoperatif sorunlara özel dikkat gösterilmelidir. Tutarsızlıklar teşhisin konulmasını kolaylaştırabilir (Dr.Ertan BEYATLI).
Çalışma Yöntemi
Laboratuvar çalışmaları
Postkolesistektomi Sendromu (PKS) için yapılan çalışmalardaki ilk laboratuvar çalışmaları genellikle şunları içerir:
- Enfeksiyöz etyolojilerini taramak için tam kan sayımı (CBC)
- Pankreas hastalığı için taranacak temel metabolik panel (TMP) ve amilaz seviyesi
- Karaciğer veya safra yolları hastalıklarında tarama için karaciğer fonksiyon paneli (HFP) ve protrombin zamanı (PT)
- Hastanın akut olarak hastalığı varsa, kan gazı analizi
Laboratuvar bulguları referans aralıklardaysa, belirtilerin bulunduğu zaman bu çalışmaları tekrar etmeye dikkat edilmelidir (önemli!!)
Diğer laboratuvar çalışmaları aşağıdaki gibidir:
- lipaz
- Gama-glutamil transpeptidaz (GGT)
- Hepatit paneli
- Tiroid fonksiyonu
- Kardiyak enzimler
Radyografi
Alt akciğer, diyafram ve mediastinal hastalıkları taramak için göğüs radyografisi yapılmalıdır; Çoğu durumda abdominal filmler de elde edilmelidir. Sırt problemleri veya artrit öyküsü olan hastalarda, daha düşük dorsal omurga serisi de edinilmelidir. Sağ üst kadran ağrısı olan hastalar için gastroözofageal reflü hastalığı (GERD) ve peptik ülser dahil olmak üzere özofajit bulguları için barsak yolunu, baryum swallow (ÖMD), üst gastrointestinal (GI) ve ince barsak takibi (SBFT) çalışmaları değerlendirecektir.
Bu çalışmalar her zaman uygulanmaz, çünkü endoskopi (özofagogastroduodenoskopi) bu hastalıkların belirlenmesinde daha güvenilirdir ve aynı zamanda Vater ampülünün doğrudan görselleştirilmesine izin verir. Karında ağrı daha düşük olduğunda, baryumlu bir lavman yapılmalıdır. Ayrıca bazı durumlarda örneğin koroner veya bağırsak anjini gibi vasküler rahatsızlıklarda anjiyografi yapılabilir.
Ultrasonografi
Ultrasonografik bir çalışma neredeyse her zaman yapılır; karaciğer, safra yolları, pankreas ve çevresi değerlendirmek için hızlı, noninvaziv ve nispeten ucuz bir yoldur. Ortak safra kanalının (CBD) 10 ila 12 mm’lik bir genişlemesi yaygın şekilde gözlenir. 12 mm’yi aşan dilatasyon genellikle engellenmiş bir taş, MİD daralması veya ampullik stenozu gibi distal obstrüksiyonunu gösterebilir.
PKS’li 80 hastayı içeren bir çalışmada, Filip ve arkadaşları, endoskopik ultrasonografinin (EUS), hangi hastaların ERCP (endoskopik retrograd kolanjiyopankreatografi) gerektirdiğini belirlemede değerli bir araç olduğuna karar vermişlerdir. EUS’un sensitivitesi ve özgüllüğü sonuç olarak safra veya pankreatik hastalık tanısı konan 53 hastanın alt grubunda sırasıyla %96.2 ve %88.9 olarak bulundu. Araştırmacılar, EUS kullanımının, ERCP alan hastaların sayısını% 51 azaltmaya yardımcı olduğunu buldu.
Endoskopi ve Kolonoskopi
Endoskopi PKS çalışmalarında çok yardımcı olabilir. Yemek borusundan duodenum yoluyla hastalık belirtileri için mukozayı değerlendirmek için iyi bir prosedürdür. Endoskopi ayrıca ampulla of Vateri doğrudan görüntülemesine izin verir. Endoskopi hakkında daha detaylı bilgi için buradaki makaleme göz atabilirsiniz (bkz; Endoskopi, Dr.Ertan BEYATLI). Total kolonoskopi koliti ortaya çıkarabilir ve terminal ileumun biyopsisi Crohn hastalığını doğrulayabilir.
ERCP (Endoskopik Retrograd Kolanjiopankreatografi)
ERCP, PKS tanısında en faydalı testtir.
Ampulla, biliyer ve pankreatik kanalların görüntülenmesinde eşsizdir. PKS’li hastaların en az %50’sinde safra yolları hastalığı vardır ve bu hastaların çoğunun şartları işlevsel niteliktedir. Tecrübeli bir endoskopist bu hastaların çoğunda bu tanıyı teyit edebilir ve ayrıca biliyer ve ampuller manometri gibi ek tanısal çalışmalar sağlayabilir. Gecikmeli boşaltma, ERCP sırasında ve ayrıca hepatoiminodiasetik asit (HIDA) taraması sırasında gözlemlenebilir. CBD, 45 dakika içinde kontrastdan uzak durmalıdır.
Biliyer manometri, narkotiksiz sedasyonlu hastalarda perfüzyon kateteri ile gerçekleştirilir; sfinkter manometresi için çekme tekniği kullanılır. Sfinkter 5-10 mm uzunluğundadır ve normal basınçlar 30 mmHg’den düşüktür. Teknoloji ilerledikçe, geriye doğru kasılmaları veya artmış kasılmaların sıklığını (takyoidi olarak da adlandırılır) tespit etmek daha kolay olacaktır. ERCP ile Oddi sfinkteri stenozu içindilatasyon, taş ekstraksiyonu, striktür dilatasyonu veya sfinkterotomi gibi terapötik manevralar yapılabilir. Perkütan transhepatik kolanjiyografi (PTC) veya manyetik rezonans kolanjiopankreatografi (MRCP), ERCP için aday olmayan ya da ERCP’ye başarısız girişimde bulunan hastalarda yararlı olabilir. (ERCP hakkında daha detaylı bilgi için buradaki makaleme göz atabilirsiniz ERCP: nedir ve nasıl yapılır?)
BT ve MR
Bilgisayarlı tomografi (BT), alkolik hastalarda veya pankreatit öyküsü olanlarda kronik pankreatit veya psödokistlerin saptanmasında yardımcı olabilir. Endoskopi ve ERCP için aday olmayan hastalarda, helikal BT taraması veya MRCP, PKS’nin nedenini ortaya koyabilir.
Nükleer Görüntüleme
Nükleer görüntüleme postoperatif safra sızıntısı gösterebilir. Bazen bir HIDA taraması veya benzeri bir sintigrafi çalışması, boşaltılmayı geciktirmeyi veya uzun süren bir yarılanma zamanını gösterebilir. Ancak bu çalışmalar, genişleme, striktür vb. tanımlamak için gerekli olan çözünürlüğe sahip değildir. İki saatten fazla geciktirilen boşaltma veya uzun süren bir yarı zamanlı olay, Oddi sfinkterinin potansiyel bir neden olarak belirlenmesine yardımcı olabilir, ancak stenoz ile diskinezi arasındaki farkı ayırt edemez.
Diğer Testler
Eski kayıtların incelenmesi, fizik muayenesi ve gözden geçirilmesine ek olarak, koroner hastalığı taramak için elektrokardiyografi (EKG) yapılmalıdır. Bir stres testi veya Holter izlemesi, geçmişin bulguları, fiziksel, laboratuvar testleri veya EKG ile belirtilebilir. Ağrı için morfin-neostigmin testi veya pankreatik kanal dilatasyonu için sekretin stimülasyon testi gibi provokasyon testleri yaygın şekilde kabul görmemiştir.
Tedavi Aşaması
Yaklaşım Hususları
Postkolesistektomi Sendromu (PKS) genellikle geçici bir tanıdır. Birçok hastada tam bir çalışmadan sonra organik veya fonksiyonel bir tanı konur. Bir tanı konduktan sonra, tedavi, o tanı için belirtildiği şekilde devam etmelidir. Tedavi tıbbi veya cerrahi olabilir. Dr Ertan BEYATLI
Farmakolojik Terapi
İrritabl bağırsak sendromlu hastalar hacim arttırıcı ajanlar, antispazmodikler veya sakinleştiricilerden yararlanabilir. İrritabl sfinkter, yüksek dozda kalsiyum kanal blokerlerine veya nitratlara cevap verebilir; ancak mevcut kanıtlar henüz inandırıcı değildir. Kolestiramin tek başına ishal olan hastalar için yararlı olmuştur. Antasitler, histamin 2 (H2) blokörleri veya proton pompa inhibitörleri (PPI’ler) bazen gastroözofageal reflü hastalığı (GÖRH) veya gastrit semptomları olan hastalar için rahatlama sağlayabilir. Bir çalışma lovastatinin hastaların %67’sinde en azından biraz rahatlama sağlayabileceğini gösterdi.
Cerrahi müdahale
Medikal tedavi gibi, cerrahi tedavi de spesifik tanıya yönlendirilmelidir. [Dr.Ertan BEYATLI]. Ameliyattan iyi yanıt alınacağı tespit edilen durumlarda elbette cerrahi müdahale yapılabilir. En sık uygulanan prosedür hem diagnostik hem de terapötik olabilen endoskopik retrograd kolanjiopankreatografi (ERCP) ‘dir. Keşif cerrahisi (tanısal diagnostik girişim), tanı almayan ve tıbbi tedaviye dirençli olan hastada son çare olabilir.
1947’de Womack, skarın ve sinir dokusunun kistik kanal kütüğü etrafında rezeksiyonunu önerdi; ancak bu yöntem biraz tartışmalı. Diğerleri nöroma, kistik kanal kalıntısı, sfinkter dilatasyonu, sfinkterotomi, sfinkeroplasti, safra yolu bypass, ortak safra kanalı (CBD) araştırması ve taş çıkarmayı önerdi. ERCP ile bu teşhislerin çoğu reddedilmiş veya tedavi edilmiş ve nöromanın kesilmesi fikri tartışmalıdır.
Alkol veya uyuşturucu kullanılan hastaların tedavisi özellikle zordur ve bu ilaçların kötüye kullanılmasına son verilmesine kadar tanısal müdahale ertelenmelidir. Bazı hastalarda neden saptanmaz, ancak durum safra ve pankreatik kanallar da dahil olmak üzere sfinkteroplastiye yanıt verebilir. Bu hasta grubu preoperatif olarak henüz tanımlanamamıştır.
Tam bir değerlendirmeden sonra (sfinkterotomiyle birlikte ERCP dahil olmak üzere) hastada zayıflama, aralıklı sağ üst karın ağrısı devam ederse ve tanı konulmazsa normal bir tanısal laparotomi sonrası transduodenal sfinkteroplasti tercih edilebilir. Safra yollarına düşen veya kalıntı taşlar için genelde ERCP yeterli olur. Ancak, bazı durumlarda bu taşların cerrahi eksiyonu gerekebilir.Dr.Ertan BEYATLI