Spinal anestezi, subaraknoid boşluğa ince bir iğneyle lokal anestezik veya opioid enjekte edilmesini içeren bir bölgesel anestezi şeklidir. İğne, genellikle 9 cm uzunluğundadır.
Ayrıca spinal blok, subaraknoid blok, intradural blok ve intratekal blok olarak da adlandırır. Latincede Spinal anaesthesia (kısaltması SP).
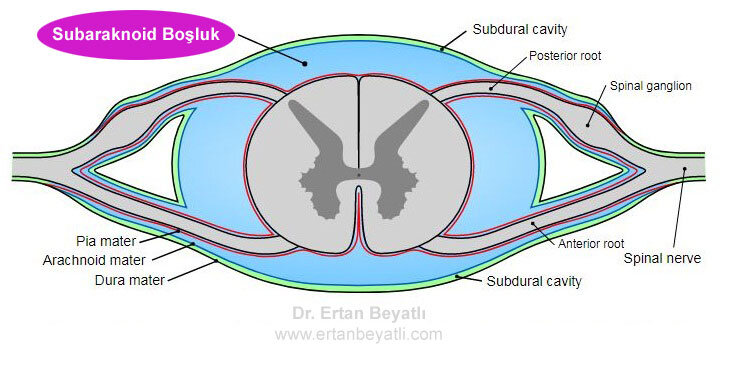
Subaraknoid boşluk, normalde araknoid ile pia mater arasında bulunan ve beyin omurilik sıvısı ile dolu olan ve omuriliğe kadar devam eden boşluktur.
Bu anestezi türü göbek altı ameliyatlarında tercih edilen güvenli ve etkili bir anestezi şeklidir. Beyin omurilik sıvısına (BOS) enjekte edilen opioid içeren veya içermeyen lokal anestetik, lokorejyonel anestezi sağlar (yani gerçek analjezi, motor, duyusal ve otonomik – sempatik blokaj). Beyin omurilik sıvısında lokal anestezik olmadan analjeziklerin (opioid, alfa2-adrenoreseptör agonisti) uygulanması, lokorejyonel analjezi üretir (yani azalmış ağrı hissi, biraz otonomik – parasempatik blokaj), ancak duyusal veya motor blok yok. Lokorejyonel analjezi, özellikle motor ve sempatik blok olmaması nedeniyle bazı postoperatif bakım ortamlarında lokorejyonel anesteziye tercih edilebilir.
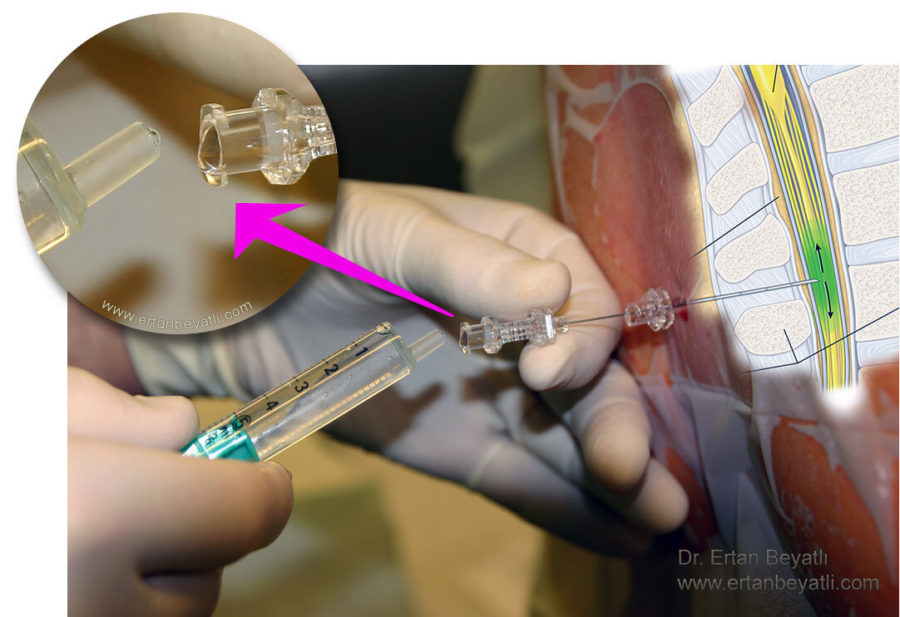
Spinal iğnenin ucunda küçük bir eğim vardır. Son zamanlarda kalem uçlu iğneler kullanıma sunulmuştur (Whitacre, Sprotte, Gertie Marx ve diğerleri).
- İndikasyonlar (Belirteçler)
- Kontrendikasyonlar
- Riskler ve komplikasyonlar
- Nasıl Yapılır?
- Epidural ve Spinal anestezi arasındaki farklılıklar
- Spinal anestezinin Tarihçesi
İndikasyonlar (Belirteçler)
Spinal anestezi, tek başına veya sedasyon veya genel anestezi ile kombinasyon halinde yaygın olarak kullanılan bir tekniktir. En yaygın olarak göbek altı ameliyatlarında kullanılır, ancak son zamanlarda kullanımı göbek üstü bazı ameliyatlara ve postoperatif analjeziye kadar uzanmıştır. Spinal anestezi kullanan prosedürler şunları içerir:
- Oropedi: Artroplasti ve eklem protezi dahil pelvis, kalça, femur, diz, tibia ve ayak bileğinde ortopedik cerrahi
- Kalp ve Damar:
- Bacaklarda damar cerrahisi
- Endovasküler aort anevrizma onarımı
- Genel Cerrahi:
- Fıtıklar (Göbek Fıtığı, kasık veya epigastrik herniler)
- Hemoroid işlemleri: Hemoroidektomi, Lazer hemoroid tedavisi
- Üroloji vakaları
- Genel anestezi ile birlikte nefrektomi ve sistektomi
- Prostatın transüretral rezeksiyonu (TUR) ve mesane tümörlerinin transüretral rezeksiyonu
- Kadın hastalıkları
- Kullanılan farklı tekniklerde histerektomi
- Sezaryen ameliyatları
- Vajinal doğum ve doğum sırasında ağrı yönetimi
- Anestezi altında muayeneler
Spinal anestezi, genel anestezi ve başarısız entübasyon riskini ortadan kaldırdığı için sezaryen için tercih edilen tekniktir. Aynı zamanda annenin bilinçli olduğu ve eşin çocuğun doğumunda mevcut olabileceği anlamına gelir. Steroid olmayan antienflamatuvar ilaçlara ek olarak intratekal opioidlerden gelen ameliyat sonrası analjezi de iyidir.
Spinal anestezi, cerrahi bölge spinal blokaj için uygun olduğunda, KOAH gibi ciddi solunum hastalığı olan hastalar için entübasyon ve ventilasyonun olası solunumsal sonuçlarını önlediği için uygun bir alternatiftir. Anatomik anormalliklerin trakeal entübasyonu çok zorlaştırabildiği hastalarda cerrahi bölge spinal blokaja uygun olduğunda da yararlı olabilir.
Pediyatrik hastalarda spinal anestezi özellikle zor hava yolları olan çocuklarda ve artan solunum riskleri veya tok mide varlığı gibi endotrakeal anestezi için kötü adaylar olanlarda yararlıdır.
Bu aynı zamanda ameliyat sonrası ağrıyı, özellikle torasik, abdominal pelvik ve alt ekstremite ortopedik prosedürlerini etkili bir şekilde tedavi etmek ve önlemek için kullanılabilir.
Kontrendikasyonlar
Spinal anestezi almadan önce, mutlak bir kontrendikasyon olmadığından emin olmak ve riskleri ve komplikasyonları en aza indirmek için kapsamlı bir tıbbi değerlendirme yapmak önemlidir. Kontrendikasyonlar nadir olmakla birlikte aşağıda bazıları verilmiştir:
- Kişinin kabul etmemesi, Hasta reddi
- Belde enjeksiyon yerinde lokal enfeksiyon veya sepsis
- Kanama bozuklukları, trombositopeni veya sistemik antikoagülasyon (artmış spinal epidural hematom riskine ikincil)
- Şiddetli aort darlığı
- Artmış kafa içi basıncı
- Beynin yer kaplayan lezyonları
- Omurganın anatomik bozuklukları
- Hipovolemi, örneğin obstetrik hastalar dahil, masif kanamadan sonra
- Alerji
- Özel durumlar (tartışmalı): Ehlers Danlos Sendromu veya lokal anesteziye dirence neden olan diğer bozukluklar
Riskler ve komplikasyonlar
Spinal anestezinin komplikasyonları sinir sistemi üzerindeki fizyolojik etkilerden kaynaklanabileceği gibi yerleştirme tekniğiyle de ilgili olabilir. Yaygın yan etkilerin çoğu küçük çaplıdır ve kendi kendine çözülür veya kolayca tedavi edilebilirken, büyük komplikasyonlar daha ciddi ve kalıcı nörolojik hasara ve nadiren ölüme neden olabilir. Bu semptomlar, anestezi uygulamasından hemen sonra ortaya çıkabilir veya ameliyattan 48 saat sonra ortaya çıkabilir.
Yaygın ve küçük çaplı komplikasyonlar şunları içerir:
- Hafif hipotansiyon
- Kalbin yavaşlaması (Bradikardi)
- Bulantı ve kusma
- Geçici nörolojik semptomlar (bacaklarda ağrı ile birlikte bel ağrısı)
- Dural ponksiyon sonrası baş ağrısı veya spinal baş ağrısı – Kullanılan spinal iğnenin boyutu ve tipi ile ilişkilidir. 2020 meta analizi, PDDH riskini azaltmak için 26-G atravmatik hipodermik iğnenin kullanılması önerildiği sonucuna varmıştır.
Ciddi ve kalıcı komplikasyonlar nadirdir ancak genellikle kardiyovasküler sistem ve nörolojik sistem üzerindeki fizyolojik etkilerle veya enjeksiyonun kasıtsız olarak yanlış yerde olmasıyla ilgilidir. Aşağıdakiler bazı önemli komplikasyonlardır:
- Sinir yaralanmaları: Cauda equina sendromu, radikülopati
- Kalp durması (kardiyak arrest)
- Şiddetli hipotansiyon
- Spinal sinirlerin sıkışmasına bağlı sonradan nörolojik sekel olan veya daha önce var olmayan spinal epidural hematom.
- Epidural apse
- Enfeksiyon (ör. Menenjit)
Nasıl Yapılır?
Kullanılan ilaç (anestezik ajan) ne olursa olsun istenen etki, afferent sinir sinyallerinin periferal nosiseptörlerden iletilmesini engellemektir. Vücuttan gelen duyusal sinyaller engellenerek ağrıyı ortadan kaldırır. Nöronal blokaj derecesi, kullanılan lokal anestezik miktarına ve konsantrasyonuna ve aksonun özelliklerine bağlıdır. Ağrıyla ilişkili ince miyelinsiz C-lifleri önce bloke edilirken kalın, ağır miyelinli A-alfa motor nöronları orta derecede bloke edilir. Ağır miyelinli, küçük preganglionik sempatik lifler en son bloke edilir. İstenen sonuç, bölgenin toplam uyuşmasıdır. Dolayısıyla hastalar ameliyat sırasında ağrıyı hissetmese de dokulara uygulanan baskıyı biraz algılayabilir (kalın A-beta mekanoreseptörlerinin eksik blokajı nedeniyle). Bu, ameliyatı geçiren kişiye hiçbir acı hissi vermeden cerrahi işlemlerin yapılmasına izin verir.
İşlem sırasında hastanın gevşemesine ve vakit geçirmesine yardımcı olmak için bazen bir miktar sedasyon sağlanır ancak başarılı bir spinal anestezi ile ameliyat hasta tamamen uyanıkken yapılabilir.
- Anatomi
Spinal anestezide iğne dura materin ötesinde bulunan subaraknoid boşlukta ve bel omurları arasına yerleştirilir. Bu boşluğa ulaşmak için, iğnenin birkaç doku ve bağ katmanını delmesi gerekir (supraspinöz ligament, interspinöz ligament ve ligamentum flavum). Omurilik (Spinal cord veya conus medullaris) tipik olarak omurganın L1 veya L2 seviyesinde olduğundan, omuriliğin yaralanmasını önlemek için iğne bunun altına L3 ve L4 boşluğu veya L4 ve L5 boşluğu arasına yerleştirilir.
- Pozisyon (Konumlandırma)
Hastanın konumlandırılması prosedürün başarısı için çok önemlidir ve ilacın nasıl yayıldığını etkileyebilir. Kullanılan 3 farklı pozisyon vardır: oturma, yana dekübit ve yüzüstü. Oturma ve yan dekübit pozisyonları en yaygın olanıdır.
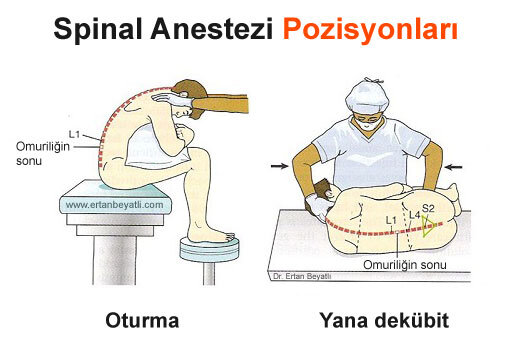
Oturma – Hasta, muayene masasının kenarında, sırtı sırtı dönük ve bacakları masanın ucundan sarkacak ve ayakları bir tabure üzerinde duracak şekilde dik oturur. Hasta omuzlarını öne çıkararak sırtına kambur şekli verir.
Lateral dekübitus- Bu pozisyonda hasta, sırtını yatağın kenarında dönük olacak şekilde yan yatırılır. Hasta omuzlarını ve bacaklarını kıvırmalı ve sırtının altını bükmelidir (cenin pozisyonu)
Yüzüstü: Hasta yüzükoyun yatar ve sırtı yukarı bakar. - Sınırlamalar
Spinal anestezi tipik olarak göbek hizasına kadar yapıları içeren ameliyatlarda uygulanır. Daha yüksek seviyelere uygulanırsa solunum ve kalp işlevlerini etkileyebilir (interkostal solunum kaslarını ve hatta diyaframı felç edebilir, kalp atışını yavaşlatabilir ve kalbi durdurabilir). Ayrıca, L1 seviyesinden daha yüksek spinal anestezi enjeksiyonu omuriliğe zarar verebilir ve bu nedenle genellikle yapılmaz.
- Enjekte edilen maddeler
Bupivakain (Marcaine) en yaygın kullanılan lokal anesteziktir, ancak lidokain (lignokain), tetrakain, prokain, ropivakain, levobupivicaine, prilocaine veya cinchocaine de kullanılabilir. Bloğu iyileştirmek ve ameliyat sonrası ağrının giderilmesini sağlamak için yaygın olarak opioidler eklenir, örnekler arasında morfin, fentanil, diamorfin ve buprenorfin bulunur. Analjezinin süresini uzatmak için klonidin veya epinefrin gibi non-opioidler de eklenebilir (Klonidin hipotansiyona neden olabilir). Avrupa ülkelerinde, 2004’ten beri Ulusal Sağlık ve Bakım Mükemmelliği Enstitüsü, sezaryen için spinal anestezinin intratekal diamorfin ile desteklenmesini önermektedir ve bu kombinasyon şu anda bu endikasyon için modal anestezi formudur. ABD’de klinik uygulamada diamorfin (eroin) kullanılmadığından, morfin aynı amaçla sezaryenlerde kullanılmaktadır.
Barisite (Baricity), insan beyin omurilik sıvısının yoğunluğu ile karşılaştırıldığında bir maddenin yoğunluğunu ifade eder. Barisite, anestezide, belirli bir ilacın intratekal boşlukta nasıl yayılacağını belirlemek için kullanılır. Genellikle, hiperbarik (örneğin, hiperbarik bupivakain), hastayı eğerek Anesteziyolog tarafından etkili ve öngörülebilir şekilde kontrol edilebildiğinden seçilir. Hiperbarik solüsyonlar, karışıma glikoz eklenerek daha yoğun hale getirilir.
Epidural ve Spinal anestezi arasındaki farklılıklar

Epidural anestezi, ilacın (anestezi ajan) epidural boşluğa yerleştirilen bir kateterden enjekte edildiği bir tekniktir. Bu teknik spinal anesteziye benzer ancak aralarında bazı farklılıklar mevcuttur. Şöyle:
- Spinal anestezide ilaç subaraknoid boşluğa yani beyin omurilik sıvısına (BOS) enjekte edilir. Dolayısıyla, doğrudan omurilik üzerinde etki etmesini sağlar. Epidural anestezide ise ilaç dura dışına (BOS dışı) verilir ve asıl etkisi durayı epidural seviyesinde terk eden sinir kökleri üzerinde olur.
- Spinal anestezide, enjeksiyon seviyesinin altında tüm motor ve duyusal fonksiyonların derin bir şekilde bloke edilmesini sağlarken, epidural anestezide, yukarıda normal fonksiyonla ve bloke edilen seviyelerin altında normale yakın fonksiyonla, enjeksiyon bölgesi çevresindeki sinir köklerini bloke eder.
- Spinal anestezide kullanılan ilaç miktarı düşüktür (1.5-3.5 mL). Epidural anestezide ise enjekte edilen ilaç dozu daha büyüktür (10-20 mL).
- Spinal anestezi sadece tek seferlik yapılır. Epidural anestezide ise enjeksiyonların yeniden yapılmasına izin veren kalıcı bir kateter yerleştirilebilir. Bu nedenle spinal anestezi kısa işlemler için daha sık kullanılır.
- Spina anestezinin etkisi 5 dakikada başlarken, bu süre epiduralde yaklaşık 25-30 dakikadır.
- Epidural, spinal kadar önemli bir nöromüsküler bloğa neden olmaz.
- Spinal anestezi genellikle bel kısmına (L2’nin altına) yapılır. Epidural anestezi ise boyun (servikal), göğüs (torasik) ve bel (lomber) bölgelerine yapılabilir.
Spinal anestezinin Tarihçesi
İlk spinal analjezi 1885’te New York’ta bir nörolog olan James Leonard Corning (1855–1923) tarafından uygulanmıştır. Dura mater’ı kazara deldiğinde bir köpeğin omurga sinirleri üzerinde kokainle deneyler yapıyordu.
İnsanda ameliyat için planlanan ilk spinal anestezi, August Bier (1861-1949) tarafından 16 Ağustos 1898’de, 34 yaşındaki bir işçiye 3 ml %0.5 kokain solüsyonu enjekte ettiği Kiel’de uygulandı. 6 hastada kullandıktan sonra, kendisi ve asistanı omurgalarına kokain enjekte etti. Bu yöntemi bacak ameliyatları için önerdiler, ancak kokain toksisitesi nedeniyle daha sonra vazgeçtiler.
Yararlanılan Kaynaklar
Cwik, Jason (2012). “Postoperative Considerations of Neuraxial Anesthesia”. Anesthesiology Clinics. 30 (3): 433–443. doi:10.1016/j.anclin.2012.07.005. PMID 22989587.
Bier A. Versuche über Cocainisirung des Rückenmarkes. Deutsch Zeitschrift für Chirurgie 1899;51:361. (translated and reprinted in ‘Classical File’, Survey of Anesthesiology 1962, 6, 352)
Liu, Spencer; McDonald, Susan (May 2001). “Current Issues in Spinal Anesthesia”. Anesthesiology. 94 (5): 888–906. doi:10.1097/00000542-200105000-00030. PMID 11388543.
https://en.wikipedia.org/wiki/Spinal_anaesthesia#:~:text=Spinal%20anaesthesia%20(or%20spinal%20anesthesia,cm%20(3.5%20in)%20long.