Meme kanseri, süt bezleri veya sütü meme başına taşıyan kanalları döşeyen hücrelerden gelişiyor. Nedeni tam olarak bilinmemekle birlikte, genetik yatkınlık oluşturan gen mutasyonu memede kanser riskini artırıyor.
Meme CA nedir?
Meme CA, memenin süt bezlerinde ve üretilen sütü meme başına taşıyan kanalları döşeyen hücreler arasında, çeşitli etkenler sonucu kontrolsüz şekilde çoğalan ve başka organlara yayılma potansiyeli taşıyan hücrelerden meydana gelen tümöral oluşumdur.
Memede kanser oluşumunda hangi etkenlerin neden olduğu kesin olarak bilinmiyor. Ancak günümüze kadar yapılan çalışmalarda, yüksek olasılık gösteren bazı faktörler belirlenmiş bulunuyor. Bazı kadınlarda genetik yatkınlık oluşturan gen mutasyonları (genlerde kansere eğilim yaratan bozukluklar) memede kanser riskini artırırken, diğerleri kadın olmak dışında bir risk faktörü taşımıyor.
Meme Kanseri ‘nde En büyük risk Kuzey Avrupalı kadınlarda
Meme kanserinden ölüm oranlarının en yüksek olduğu ülkeler Kuzey Avrupa’da bulunuyor. Bu ülkelerde oran, 100 binde 22.6. Çin ve Japon kadınların meme kanserinden ölüm oranları, Kuzey Avrupalı kadınların tam aksine, en düşük seviyede. Bu oran Çin’de 100 binde 5.6 iken Japonya’da 8.3.
ABD’de tüm yaşamı boyunca her 8 kadından biri, meme kanserine yakalanıyor. 2008 yılında ABD’de 182 binden fazla kadına malign meme tümörü yani kanser teşhisi kondu. 40 bin civarı kadın da meme kanseri nedeniyle hayatını kaybetti. Ancak bütün bu üzücü istatistiklerin yanı sıra, yüz güldüren sonuçlar da var.
Bugün ABD’de 2.5 milyon yaşayan, tedavi uygulanmış sağlıklı meme kanserli hasta bulunuyor.
40 yaş üzeri kadınlarda mamografik tarama programlarının artmasının ve menopozdaki kadınlara önerilen hormon replasman tedavilerinin gittikçe azalmasının, memede kanser tedavisindeki başarıyı artırdığı düşünülüyor.
Meme Kanseri Risk Faktörleri
Bir çok faktör rol oynamaktadır (multifaktöryel). Bu faktörlerin arasında en önemli olan hastanın meme kanseri aile öyküsü olmasıdır.
Bu guruptaki insanlar periyodik ve özel bir şekilde takip edilmelidirler. Erken dönemde teşhis edilen meme kanseri hastaları yapılacak yeterli cerrahi müdahaleden sonra normal bir yaşam sürdürmeleri söz konusudur..

- Cinsiyet. Meme kanseri en sık kadınlarda görülüyor. Erkeklerde görülme oranı, yüzde 1’den daha az.
- Yaş. çoğunlukla 50 yaş ve üzerinde görülüyor. 35 yaş ve altında rastlanma sıklığı daha az. 2000-2004 yılları arasındaki Amerikalı kadınlardaki meme kanseri insidansı 30-34 yaş grubunda 100 binde 25 iken, 45-49 yaş grubunda 100 binde 190’a ve 70-74 yaş grubunda ise 100 binde 455’e yükseliyor. Herediter (kalıtsal) meme kanseri veya genetik bozukluklar nedeniyle oluşmuş meme kanserleri genç yaşlardaki kadınlarda daha sık görülüyor.
- Aile hikayesi. Özellikle anne tarafından 1. derece akrabasında (anne, teyze, anneanne, kızı) meme kanseri hikayesi olması önemli bir risk faktörü kabul ediliyor. Bu akrabaların meme kanserine menopoz öncesi yakalanmaları ve/veya çift taraflı meme kanseri olmaları, riski daha da artıyor.
- Östrojen hormonu. Bir kadın ilk adetini ne kadar erken görürse (örneğin 12 yaştan önce) ve menopoza ne kadar geç girerse (örneğin 55 yaş), meme kanserine yakalanma riski o kadar artıyor. Doğum kontrol hapı kullanmanın da, çok düşük oranda olsa bile kanser riskini artırdığı düşünülüyor.
- Menopoz sonrası hormon tedavisi. Menopoz dönemindeki, sıcak basması gibi sorunların önlenmesi amacıyla kadın hastalıkları ve doğum uzmanlarınca uzun süreli reçete edilen (5 yıl veya daha fazla süreyle) östrojen ve medroksiprogesteron asetat içeren kombine hormon ilaçları, meme kanseri riskini sadece östrojen içeren hormon ilaçlarına kıyasla daha çok artırıyor.
- Geçirilmiş meme biyopsisi. Meme biyopsilerinde saptanan orta dereceli hiperplaziler meme kanseri riskini 1,5-2 kat (hafif derecede), atipik duktal hiperplazi 3-5 kat (orta derecede) ve lobüler karsinoma in situ (yayılma göstermeyen) veya aile hikayesi ile beraber atipik duktal hiperplazi ya da lobüler hiperplazi varlığı riski 8-10 kat (yüksek derecede) artırıyor.
- Meme kanseri hikayesi. Bir kadının bir memesinde daha önce kanser gelişmiş olması, ileride diğer memesinde de kanser gelişmesi riskini yaklaşık 2 kat artırıyor.
- Işınlanma (radyoterapi). Çocukluk çağında başka kanserler nedeniyle (lenf kanseri vb.) göğüs ışınlaması geçirenlerde, meme kanseri görülme sıklığı artıyor.
- Beslenme ve çevre faktörleri. Yağ bakımından zengin beslenme şekli ve kilo alma, özellikle menopozdaki kadınlarda meme kanseri riskini artırıyor. Alkol kullanımı (günde bir kadehten fazla) yine riski artırırken, sigaranın etkisi hala tartışılıyor. Düzenli egzersiz ve fiziksel aktiviteninse meme kanseri riskini azalttığı biliniyor.
- Genetik bozukluklar. Herediter (kalıtsal) meme kanseri genleri (BRCA1 ve BRCA2) tüm meme kanserlerinin yüzde 5-10’unu oluşturuyor.
YANLIŞ
Kişinin ailesinde meme kanseri öyküsü yoksa kanser riski yoktur.
DOĞRU
Meme kanseri olan kadınların yüzde 75’inin ailesinde meme kanseri öyküsü bulunmuyor. ‘Kadın’ olmak tek başına meme kanseri riski taşımak anlamına geliyor.
Kalıtsal Meme Kanserleri
Herediter (kalıtsal ya da ailevi) meme kanseri sendromları, meme kanserli hastaların yaklaşık yüzde 5-10’unda görülen bir durum. Kalıtsal meme kanserlerinin yüzde 80’inden sorumlu iki gen var: BRCA-1 ve BRCA-2. BRCA-1 geninde bozukluk (mutasyon) olan kadınlarda 70 yaşına dek meme kanseri gelişme riski yüzde 85, over (yumurtalık) kanseri riski ise yüzde 45. BRCA-2 gen mutasyonu taşıyıcılarındaysa, 70 yaşına dek meme kanseri riski yüzde 84 ve yumurtalık kanseri riski yüzde 76.
Tanı nasıl konuyor?
BRCA-1 ve BRCA-2 için tanı, genetik test yapılarak konuyor. Bu gruptaki kişilere, 18 yaşından itibaren meme muayenesi, 25-35 yaşında mamografi, 25-35 yaşından itibaren 6 ayda bir veya yıllık klinik meme muayenesi ve yıllık meme MR’ı öneriliyor. Ayrıca bu kişilerin, 30-35 yaşından itibaren 6 ayda bir yumurtalık kanseri için tetkiklerini aksatmamaları gerekiyor.
Hangi önlemler alınıyor?
Bu kişilere uygulanabilecek risk azaltıcı metotların başında; tamoksifen veya raloksifen gibi östrojeni baskılayan ilaçların kullanımı veya risk azaltıcı koruyucu cerrahi girişimler geliyor. Bu cerrahi girişimlerse, çift taraflı yumurtalıkların ve memelerin çıkarılması (bilateral salfingo-ooferektomi ve proflaktik bilateral mastektomi) olarak sıralanıyor. Tamoksifen ve raloksifen kullanımı, meme kanseri riskini yarı yarıya azaltıyor. Koruyucu amaçla yumurtalıkların çıkarılması bu hastalarda meme kanseri riskini yüzde 50, proflaktik mastektomi ise meme kanseri riskini yüzde 90 azaltabiliyor.
Kimler genetik danışmanlık almalı?
Özellikle kalıtsal kanserlerin sık görüldüğü Doğu ve Orta Avrupa kökenli Aşkenazi Yahudisi kadınların, birinci derece, bir veya birden fazla genç yaşta veya çift taraflı meme kanserli akrabası olan kadınların mutlaka genetik danışmanlık alması gerekiyor. Genetik danışmanlar, bu riskleri taşıyan kişileri BRCA-1 ve BRCA-2 gen mutasyon tarama testlerinin onlar için gerekli olup olmadığı, bu testlerin tıbbi ve psikososyal açıdan avantajları ile dezavantajları hakkında bilgilendiriyorlar.
Kimler risk altında?
Ailede bir veya birden fazla, birinci ya da ikinci derece akrabasında meme kanseri bulunması kalıtsal meme kanserini düşündürüyor. Bununla birlikte meme kanserinin 20-30 gibi çok genç yaşlarda özellikle yumurtalık kanseri ile birlikte görülmesi de kalıtsal meme kanserini akla getiriyor. Annede veya kız kardeşte meme kanseri bulunması ciddi bir risk faktörü kabul ediliyor.
Meme Kanseri Tipleri
Meme kanserinin çeşitli tipleri var. Ancak temel olarak iki ana gruba ayrılıyor;
- noninvazif ya da başka bir deyişle in situ (yayılma göstermeyen)
- invazif (yayılma potansiyeli olan) grup.
Noninvazif kanserler
Yayılma göstermeyen (in situ) kanserler de kendi arasında ‘duktal karsinoma in situ’ ve ‘lobüler karsinoma in situ’ olmak üzere yine iki gruba ayrılıyor. Özellikle 1980’li yıllardan sonra tarama mamografilerinin ön plana çıkmasıyla, yayılma göstermeyen (in situ) kanserlerin, tüm meme biyopsileri içindeki görülme sıklığının yüzde 1.4’ten yüzde 10’lara, tüm meme kanserleri içindeki oranlarının da yüzde 5’ten yüzde 15’lere yükselmesi dikkat çekiyor.
Klasik lobüler karsinoma in situ
Her iki memede de 8-10 kat meme kanseri riskini artıran önemli bir bulgu. Bu tür hastalara yakın izlemin yanı sıra tamoksifen gibi koruyucu bazı ilaçlar verilebiliyor veya koruyucu amaçlı her iki meme dokusunu çıkartma (basit mastektomi) şeklinde cerrahi girişimler uygulanabiliyor. Beraberinde plastik cerrahi girişimlerle meme protezi ve benzeri cerrahi rekonstrüktif işlemler eklenmesiyle beraber kozmetik açıdan yüz güldürücü sonuçlar elde edilebiliyor.
İn situ duktal kanserler (İSDK, intraduktal kanser)
Çoğu kez muayenede kendini belli etmiyor. Belirtisi; mamografide tespit edilen düzensiz ufak boyutlu kireçlenme bulgusu ve/veya (pleomorfik mikrokalsifikasyon) kanlı/şeffaf tek kanaldan memebaşı akıntısı şeklinde oluyor. İSDK, normal hücrelerden yayılma potansiyeli olan (invaziv) kanser hücrelerine geçiş olarak kabul ediliyor. Kitle oluşturmadığı için, tel ile veya radyoaktif maddelerle işaretlenerek çıkarılıyor. Eğer kanser, tek odaklı bir durumda ise etrafında yeterli temiz doku bırakılıyor.
Geri kalan meme dokusuna radyoterapi (RT) uygulandığı zaman hastalık, klinik olarak iyi bir seyir gösteriyor. Eğer memede yaygın olarak bulunuyorsa, tüm meme dokusunun çıkarılması (basit mastektomi) gerekiyor ve bu durumda yüzde 100’e varan oranla tam iyileşme görülüyor. Saf İSKD’de koltukaltı lenf bezlerinin tutulumuna nadir olarak yüzde 1-3 oranında rastlanıyor. Bu nedenle tüm memenin çıkarılacağı hastaların; daha kötü özellikler gösteren (yüksek gradlı vs.) bazı tiplerinde, koltukaltı lenf bezlerinde kanser hücrelerini tutması en muhtemel bekçi lenf bezlerini çıkarmak (sentinel lenf nodu biyopsisi) gerekebiliyor.
İnvaziv kanserler
Sütü memebaşından dışarı taşıyan meme kanallarını döşeyen hücrelerde gelişen duktal karsinom en sık rastlanan meme kanseri tipi. Bu da yayılma özelliğine göre ayrılıyor: Duktal karsinomun yayılma özelliği yoksa in situ formda, yayılma potansiyeli varsa invaziv formda olduğu biliniyor.
Süt üreten bezlerden (lobül) gelişen kanser lobüler karsinom olarak adlandırılıyor. Lobüler karsinom da yayılma özelliğine göre ikiye ayrılıyor. Yayılma özelliği yoksa in situ formda yayılma potansiyeli varsa invaziv formda oluyor.
İnflamatuvar meme kanseri
Meme kanserinin en kötü ve hızlı seyreden tipi olarak kabul ediliyor. Memeyi tamamen saran memenin iltihabi hastalıklarıyla karışabiliyor. Kitle belirtisi vermeden yaygın kızarıklık ve sertlikle seyrediyor. Antibiyotik tedavisine rağmen iyileşmeyen memenin iltihabi hastalıklarında mutlaka meme kanserinin akla getirilmesi ve biyopsi alınması gerekiyor.
Meme Kanseri ‘nin Belirtileri nelerdir
Meme içinde kanserleşen bir hücrenin, bir tümör oluşturması ve bir uzmanın muayene sırasında anlamasına ya da radyolojik incelemede belli olmasına kadar hayli uzun zaman geçmesi gerekiyor. Kadınlar genellikle en az 1 cm. büyüklüğüne ulaşmış bir kitleyi, elle kontrol yöntemi sayesinde fark edebiliyorlar. Günümüzde meme kanserlerinin çoğu kişinin kendisi tarafından bulunuyor.
Kanserli kitleler nispeten sert, düzensiz kenarlı, yüzeyi pürtüklü görünüyor ve meme dokusu içinde rahatça oynatılamıyor. Kanser uzak organlara metastaz (yayılım) yapmışsa bu yayılımlar, nadiren meme kanserinin ilk bulgusunu oluşturuyor. Meme kanserinin sıkça yayılma gösterdiği bölgeler ise kalça ve omurga kemikleri ile akciğer ve karaciğer.
Ancak bazı hastalarda bu belirtilerin hiçbirisi olmuyor ve meme kanseri yalnızca, mamografi incelemesiyle tespit edilebiliyor. Aşağıdaki belirtilerden en az biri varsa, vakit geçirmeden uzmana başvurulması gerekiyor.
- Memede veya koltuk altında ele gelen kitle (sertlik, şişlik)
- Meme başından akıntı (tek kanaldan kanlı veya şeffaf renkli)
- Meme başında içe doğru çekilme, çökme veya şekil bozukluğu
- Meme başı derisinde değişiklikler (soyulma, kabuklanma)
- Meme cildinde yara veya kızarıklık
- Meme cildinde ödem, şişlik ve içe doğru çekintiler olması (portakal kabuğu görünümü) (ilgili makale: Ödem nedir?)
- Memede büyüme, şekil bozukluğu veya asimetri ya da renginde değişiklik (kızarıklık vs.)

Tüm kanser türlerine bağlı ölümler arasında, meme kanserine bağlı ölümler, ikinci sırada yer alıyor. İlk sırada, akciğer kanseri bulunuyor. Türk İstatistik Kurumu (TUİK) 2007 verilerine göre, 70 milyonu aşan ülkemizde, 100 bin kadından 22’si meme kanserine yakalanıyor. Meme kanserinden ölüm oranı 100 bin kadında yaklaşık 10 kişi olarak belirtiliyor. (http://www.tuik.gov.tr)
YANLIŞ –Meme kanseri genç kadınlarda görülmez
DOĞRU –Meme kanseri 50 yaş üstü kadınlarda daha yaygın ancak her yaş kadında ortaya çıkabiliyor.
Meme Kanserinin Tanı ve Evreleri
Meme Kanserinin Tanı Yöntemleri
- Mamografi
- Ultrasonografi (meme USG)
- MR
- Meme Biyopsisi
Meme Kanserinin Evreleri
Kanser tedavisini belirleyebilmek için, hastalığın evresininin bilinmesi gerekir. Hastalığın evresi, tümörün boyutu ve ne kadar yayıldığıyla ilgilidir. Evrelendirmede, kanserin yayılıp yayılmadığını, yayıldıysa vücudun hangi bölgelerine yayıldığını öğrenmek için röntgen ve laboratuvar testlerinden yararlanılır.
Meme kanseri genellikle ilk olarak koltuk altı lenf bezlerine (axillary lymph nodes) yayılır. Kanserin boyutu, çoğunlukla, memedeki tümörün ve koltukaltındaki lenf bezlerinin ameliyatla alınmasına kadar bilinmez.
Meme kanseri tanısı konan hasta doktorunun şu soruları yanıtlamasını isteyebilir.
- Benimki ne tür bir meme kanseri?
- Hormon reseptör testi ne gösterdi? Tümör dokusunda başka hangi laboratuvar testleri yapıldı ve ne gözüktü?
- Hastalık hangi safhada? Kanser yayılmış mı?
- Bu bilgi tedavimi nasıl yönlendirecek?
Meme Kanseri kaç evreden oluşur

- Evre 0: carcinoma in situ
- Evre-1: Tümör boyutu <2 cm
- Evre-2: Tümör boyutu 2 – 5 cm
- Evre-3: Tümör boyutu >5 cm den büyük olmasıdır ya da 5 cm.’den küçük tümör olup Lenfnodu (LN) ve/veya lokal metastaz olması
- Evre-4: ise meme kanserinin başka organlara sıçramış olması (distal metastaz)
Evre 0 ‘a carcinoma in situ denir.
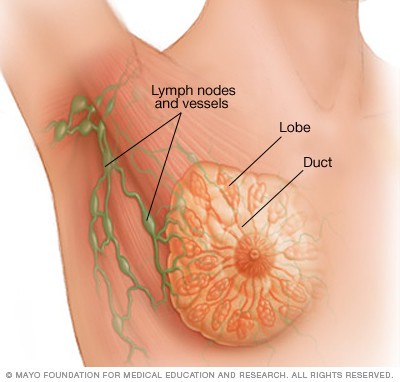
Lobüler carcinoma in situ (LCIS) lobüldeki anormal hücrelere karşılık gelir. ( Lobülün arka plan bölümünde resmini görebilirsiniz.) Bu anormal hücreler, yüksek riskin işaretçisidir. ve LCIS olan hastanın, ilerde her iki memesinde de yayılabilen kanser olma riskinin yüksek olduğu anlamına gelir (İki meme de risk altındadır).
Ductal carcinoma in situ (DCIS) kanaldaki kanser öncesi durumdur. DCIS aynı zamanda intraductal carcinoma olarak da adlandırılır. Anormal hücreler, kanalın dışına çıkıp etrafındaki meme dokusuna yayılmamıştır. Fakat bazen, DCIS tedavi edilmezse, yayılabilen kanser oluşabilir. Bu resim, erken evre meme kanserini ductal carcinoma in situ gösteriyor.

Evre I, yayılabilen meme kanserinin başlangıç safhasıdır. Bu evrede tümör boyutu 2 cm. den geniş değildir ve kanser hücreleri memeden başka yere (lenf bezlerine) yayılmamıştır.
Bu resim, kanserin kanalın dışına sıçradığı ve yakındaki meme dokusuna yayıldığını gösteriyor.
Aşağıdaki durumların her biri Evre II safhasıdır.
– Memedeki tümörün çapı 2 cm. den küçük ancak kanser koltuk altındaki lenf bezlerine sıçramış.
– Tümörün çapı 2- 5 cm. arasında ve kanser koltukaltına sıçramış.yada sıçramamış.
– Tümör 5 cm.den büyük ama koltukaltındaki lenf bezlerine sıçramamış.
Evre III A ve B olarak ayrılır:
Evre III A, memedeki kanserin çapının 5 cm.den küçük olduğu ve koltukaltındaki lenf bezlerine ve çevredeki dokuya yapıştığı ya da tümör çapının 5cm. den fazla ve koltuk altındaki lenf bezlerine yayılmış olduğu durumdur.
III B evresi, tümörün göğüs duvarına veya meme derisine doğru büyümüş veya göğüs kemiğinin (sternum) altındaki lenf bezlerine yayılmış olduğu durumdur.
Inflamatuvar meme kanseri, III B evresindeki meme kanserinin bir tipidir. Çok nadir görülür. Meme derisi kızarır ve şişer, çünkü kanser hücreleri meme derisinin lenf kanallarını tıkamıştır.
– Evre III C: Kanserin göğüs kemiğinin altındaki ve koltukaltındaki lenf bezlerine, ya da köprücük kemiğinin altındaki veya üstündeki lenf bezlerine yayıldığı durumdur. Bu evrede ilk meme tümörünün çapı önemli değildir .
Evre IV : Uzak metastatik kanserdir. Kanser vücudun diğer bölgelerine sıçramıştır.
Tekrarlayan kanser, tedaviden sonra tekrar oluşan kanserdir. Kanser, lokal (meme veya göğüs duvarında) olarak veya vücudun herhangi bir bölgesinde (kemik,karaciğer,akciğer gibi) tekrarlayabilir.
Evrelere göre tedavide başarı oranı
| Evrelere göre oran | |
| Evre 0 | %100 |
| Evre I | %98 |
| Evre II | %88 |
| Evre III A | %56 |
| Evre III B | %49 |
| Evre III C | %16 |

Meme Taramasında Kullanılan Testler
Meme taraması meme kanserinin erken tanısı için en önemli araçtır. Meme kanseri bayanlarda en sık görülen ve sedanter yaşam koşulları ile giderek artan bir kanserdir. Her 8 bayandan birisi yaşamının bir kesitinde meme kanseri hastalığına yakalanabilir. Kanser sıklığında coğrafi değişiklikler görülebilir.
1970 yılında meme kanseri tanısını daha erken koyma ve hastalara gerekli tedaviyi uygulama amacıyla Meme Taraması konusu gündeme gelmiştir. 1980 yılına gelindiğinde birçok ülkede fiilen Meme kanseri Erken tarama testleri kullanılmaya başlanmıştır.
Bu çalışmalar sonucunda meme taraması testleri ile kanserin erken dönmede tanınmasının meme kanserine bağlı ölüm risklerini azaltmada etkin olduğu tespit edilmiştir. Yapılan bazı yeni klinik çalışmalarda ölüm riskini %35 oranında azaltmanın mümkün olacağı gözlenmiştir.
Günümüzde konu hakkındaki bilimsel tartışmalar devam etse de dünyada birçok ülkede 40-50-69 yaş arasında meme kanseri taraması uygulanmaktadır.
Meme kanseri taramasında uygulanan ana yöntemler:
- kendi kendine meme muayenesi (hasta)
- klinik meme muayenesi (hekim)
- görüntüleme yöntemleri (lab.)
işte TARAMA YÖNTEMLERİ
Kendi Kendine Meme Muayenesi (Hasta Muayenesi)
Bu yöntemle hasta kendi şikayetlerine ve elle yaptığı meme muayenesini gerçekleştirir. Mememe kanserinde oluşacak şikayetler ve bulgular hakkında hekim tarafından bilgi verilmeli ve eğitim yapılmalıdır.
Kendi elinizle göğüslerinizin normal olarak nasıl hissettiğini periyodik bir şekilde kontrol edin, böylece bir şey değiştiğinde bunu fark etmeniz kolay olur.
Her ay regl döneminin 5. günü yapılması uygundur çünkü meme dokusunda daha az şişlik ve hassasiyet olur. Menopoza giren bayanlarda ise her ay aynı günlerde yapılması uygundur.
Günlük veya haftalık meme muayenesi ve kontrolü ÖNERİLMEZ.
Bunun sebebi ise yavaş büyüyen bir kitlenin gözden kaçıp fark edilmeme olasılığın yüksek olmasıdır. Bu durumu şuna benzetebiliriz. Bir filize her gün bakarsanız onun büyüdüğünü fark edemeyebilirsiniz, ya ayda bir defa bakarsanız !?
Örneğin meme boyutlarında eşitsizlik, meme ucunun çukurlaşması veya belirginleşmesi, meme cildinde portakal kabuğu görüntüsünün oluşması, meme ucundan akıntı gelmesi, koltukaltlarında ağrı şişlik veya sertlik, meme dokusunda ele gelen kitle, sertlik vb. Özellikle ağrı yapmayan meme sertliklerine (ağrısız kitle) dikkat edilmelidir. Muayene ayakta, üst beden çıplak ve ayna karşısında yapılmalıdır.

Ayakta meme muayenesi
Üst kısım çıplak bir şekildeyken aynanın karşısına geçilir. Kollar serbest bırakılır. Her iki memenin boyutu ve şekli incelenir (genelde memeler aynı boyutta olmaz bu normaldir). Ayrıca deride renk değişikliği, çukurluk, meme ucunda gömülme, vb durumlar incelenir.

Daha sonra eller kalçalara yerleştirilir ve sıkıca bastırılır. Yanlara dönerek memelerin dış bölümleri incelenir. Sonra öne doğru eğilir ve memenin dış çizgileri incelenir. Son olarak da eller ensede birleştirilir ve sıkıca kavranır ve yanlara dönerek memeler incelenir. İşaret ve başparmak ile meme ucu hafifçe sıkıştırılır ve akıntının olup olmadığı kontrol edilir.

Yatarak meme muayenesi
Sağ omuz altına bir yastık konularak yatılır. Sağ el başın arkasına alınır. Muayene için karşı elin 2, 3 ve 4. parmaklarının iç kısmı kullanılmalı ve tüm meme dairesel hareketlerle, yukarıdan aşağıya ya da dışarıdan başlayıp meme başına doğru olacak şekilde değerlendirilmelidir. Bu esnada meme dokusunu daha iyi bir şekilde hissetmek için krem veya losyon kullanılabilir.

Bu konudaki en önemli husus meme muayenesinin ayda sadece bir kez yapılmasıdır çünkü daha kısa bir sürede yapılan muayenelerde yavaş ve sinsi bir şekilde büyüyen oluşumu fark edebilmek daha zordur. Dolayısıyla bu süre kısaldıkça bulguları yakalamak daha da zorlaşabilir.
Ayrıca, bu yöntem diğer tarama ve tanı yöntemlerinin yerini alamayacağı vurgulanmalıdır ! Yani hasta “ben kendim elle baktım birşey görünmüyor hastaneye gitmeye gerek yok” dememeli ve belirli aralıklarla hekim kontrolüne gitmelidir.
Kendi kendine meme muayenesinin sensitivitesi %60, spesifisitesi %70. Bu oranlar hastanın yaşı ve sosyoekonomik durumuna göre değişebilir. Kırsal kesimdeki bir teyzenin şehirde yaşayan bir üniversite genci arasında ciddi farklılıklar olabilir !
Klinik Meme Muayenesi (Doktor Muayenesi)
Bu yöntemin erken meme kanseri tanı ve tedavi sürecinde çok önemli ve büyük rolü vardır. Muayene konu hakkında uzman hekim tarafından yapılmalıdır aksi takdirde yanlış tedavi ve tanı sürecinde gereksiz gecikmeler olabilir. Erken meme kanserini çıban veya kist zannederek takip edilen hastaların sayısı az değildir! Klinik meme muayenesinin sensitivitesi %50, spesifisitesi %95 tir (olmalıdır!).
Klinik meme muayenesi, Amerikan Kanser Derneği (ACS) tarafından 20 yaş sonrasındaki kadınlara 3 yılda bir, 40 yaşından sonraki kadınlara yılda bir olarak önerilmiştir.
Klinik meme muayenesi, meme hastalıklarının tarama, tanı ve tedavisinde; meme kanseri için risk faktörleriyle muayene bulgularını birleştiren, ciddi klinik tecrübe gerektiren önemli bir değerlendirme yöntemidir.
Mamografi ile saptanamayan ya da mamografinin meme taraması alanı içerisine girmeyen meme kanserlerinin %15’ini saptayabilmektedir. Klinik meme muayenesi özel gereç gerektirmeyen, pahalı olmayan bir yöntemidir. Bu nedenle özellikle gelişmekte olan ülkelerdeki uygulamaları önemlidir.
Görüntüleme Yöntemleri
Mammografi
Tarama mamografisi meme hastalıkları açısından asemptomatik kadınlara meme kanserinin erken tanısını sağlamak amacıyla uygulanan bir yöntemdir. İyi bir mamografi filmi memenin tamamının görüntülenmesini sağlamalıdır. Filmler hasta ayaktayken çekilir. X-ray tüpü ve kaset tutucu 180 derece dönebilen C kollu bir cihazın iki ucuna yerleştirilmiştir. Tarama mamografisinde kraniyokaudal ve mediyolataral-oblik yönlerde olmak üzere iki film çekilir.
Açıların değiştirilmesiyle, süt kalsiyumu içeren kistlerdeki sıvı seviyelerinin tanımlanması, süperpoze olmuş gölgelerle gerçek meme kitlelerinin ayırdedilmesi ve lezyonların yerinin belirlenmesi kolaylaştırılabilir. Standart iki yönlü bir mamografinin radyasyon dozu 0.25 raddır. Dijital mamografi ile film tarama mamografisinde olabilecek görüntü bozukluklarının uzaklaştırılması ve görüntüleme kalitesinin arttırılması amaçlanmaktadır.
Mamografi ile taramanın sensitivitesi %55, spesifisitesi %95 tir. Mamografi sensitivitesi yaşla birlikte artış göstermektedir. Sensitivite 40-49 yaş için %66.9, 50-59 yaş için %72.2, 60-69 yaş için %75.9 ve 70-84 yaş için %82.7 olarak saptanmıştır.
Çalışmaların uzun dönem sonuçları açıklanıp meta-analizler oluşturulduğunda mamografi ile taramanın meme kanserine bağlı mortaliteyi azaltmadaki etkinliğinin %15 olduğu sonucuna varılmıştır.
Diğer Görüntüleme Yöntemleri
Ultrasonografi, meme hastalıklarının tanısında kullanılabilen bir yöntem olmakla birlikte; kullanıcı bağımlı olduğundan ve uygulama süresi uzun vakit alabildiğinden tarama amacıyla kullanımı genellikle önerilmemektedir.31
Meme kanseri tanısında manyetik rezonans görüntüleme (MRG) kullanımı giderek yaygınlık kazanmaktadır. Manyetik rezonans görüntülemenin sensitivitesi %88-100; spesifisitesi ise %37-70 olarak bildirilmiştir. Bu nedenle malign meme hastalıklarını tanımlamadaki gücü yüksek iken; benign meme hastalıklarını da malign olarak tanımlayabilmektedir.
Fazla Şeker ve Meme Kanseri
Günlük tüketilen şeker miktarının artmasıyla birlikte sadece fazla kiloların söz konusu olmadığını ve bayanlarda memekanseri riskini ve yayılım oranını arttırdığı ortaya çıktı.

Bu çalışma Doç. Dr. Peiying Yang, PhD ve arkadaşları tarafından Texas Üniversitesi MD Anderson Kanser Merkezi’nde yapıldı ve geçtiğimiz hafta Kanser Araştırma Dergisinde (Cancer Research) yayınlandı.
Ekibin yaptığı çalışmaya göre günlük şeker alımı miktarı ile meme kanseri arasında bir ilişki bulundu ve yüksek oranla inflamasyona bağlı olduğu düşünüldü. Çalışma deneysel olarak fareler üzerinde gerçekleştirildi ve çalışmada 3 grup hayvan modeli uygulandı:
Zengin sakaroz diyet grubu, zengin fruktoz diyet grubu ve nişasta kontrol diyet grubu. Çalışmada özellikle günlük batı diyetinde mevcut olan yüksek oranda rafine şekerler, doymuş yağ ve kırmızı et ve düşük oranda taze meyve ve sebze ve tam tahıllar uygulandı.
Fazla Şeker ile Meme Kanseri riski
sakaroz açısında zengin diyet ile beslenen farelerin % 50-58’inde meme kanseri gelişti

Nişasta kontrol grubu (%30) ile karşılaştırıldığında Zengin sakaroz ve zengin fruktoz diyeti (%50-58) ile beslenen farelerde meme kanseri olasılığı anlamlı olarak daha yüksek bulundu. Ayrıca yine son iki grupta farelerin akciğerinde tespit edilen kanser hücreleri ise meme kanserinin yayılım hızının artışı ile ilgili olduğu düşünüldü.
Yapılan bu çalışmaya göre fruktoz ve sakaroz (glukoz ve fruktoz kombinasyonu) 12-lipoksijenaz (12-LOX) sinyalizasyonunu ve dolayısıyla da 12-hidroksi- 5Z, 8Z , 10E , 14z – eikosatetraenoik asit (12-HETE) seviyesini arttırarak meme kanseri riskini ve metastaz oranını yükseltmektedir.
glukoz+fruktoz → 12-LOX ↑ → 12-HETE ↑ → meme kanseri ↑
Özellikle yüksek oranda günlük sofra şekeri ve yüksek früktoz mısır şurubu tüketimi 12-HETE artışına yol açtığı MD Anderson kanser merkezinde çalışan ve bu çalışmaya katılan Prof.Dr. Lorenzo Cohen’in dikkatini çekmiştir. Ancak yüksek glukoz ve fruktoz oranının nasıl 12-LOX seviyesini yükselttiği konusundaki mekanizma henüz netlik kazanmamıştır.
Bu çalışma ABD’de yükselen şeker tüketimi (kişi başına şeker tüketimi >100kg/yıl) ile ilişkili olduğundan özellikle önemlidir.
Meme protezi kanser yapar mı?
Fransa’da nadir görülen bir kanser çeşidine neden olduğu için meme protezi yasaklandı. Fransa meme protezini yasaklayan ilk ülkedir.
Fransa Ulusal Ecza ve Sağlık Ürünleri Ajansı’ndan (ANSM: Agence nationale de sécurité du médicament et des produits de santé) yapılan bilgilendirmede, nadir görülmesine rağmen ciddi risk teşkil eden bir kanser türüne neden olabileceği için meme protezlerinin önlem babında yasaklandığı belirtildi. BBC kanalının yaptığı habere göre yasağın, altı firma tarafından üretilen pürüzlü yüzeye sahip protezler için geçerli olduğu vurguladı.
59 Meme kanser durumu saptandı, 3 hasta vefat etti
Fransa’da Meme protezi ile bağlantılı 59 kanser hastası tespit edildi, bu hastaların üçünün hayatını kaybettiği bilgisi verildi.

Meme protezi neden kanser yapar?
Meme protezlerinin dış yüzeyindeki pürüz arttıkça, bağışıklık sistemine saldıran anaplastik büyük hücreli lenfoma riskinin yükseldiği ifade edildi.
ANSM ajansı, ayrıca pürüzlü yüzeye sahip meme protezleriyle bağlantılı anaplastik büyük hücreli lenfoma vaka sayısının, 2011’den bu yana dikkat çekici biçimde arttığına işaret etti.
Sırada KANADA var
Bu kararla Fransa, pürüzlü yüzeye sahip meme protezlerini yasaklayan ilk ülke oldu. Ancak ANSM, kadınların bu protezleri çıkarmak için bir ameliyata girmeleri konusunda yorum yapmadı. ANSM, ‘riskin nadir olmasını’ buna gerekçe olarak gösterdi.
Kanada da aynı protezlerin kullanımını durdurmayı hedeflediğini açıklamıştı. Kanada, bu konuyla ilgili 28 vaka tespit ettiğini duyurmuştu.
Kaynak: Medical News Today Çeviri: Dr.Ertan BEYATLI
