Melanom, Amerika Birleşik Devletleri’nde teşhis edilen en yaygın beşinci kanserdir. 1990 yılından bu yana vaka sayısı giderek artmaktadır.
Melanom diğer bazı cilt kanserlerinden daha az yaygındır, ancak büyüme ve yayılma olasılığı daha yüksektir.
Nedenleri | Çeşitleri | Belirtileri | Teşhisi | Tedavisi
Melanom nedir?
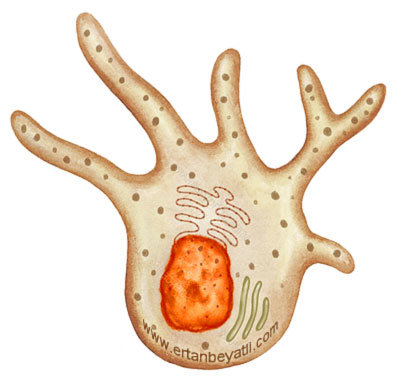
Melanom, cildin pigment hücrelerinde (melanosit) gelişen bir kanser türüdür. Melanositler, cildi ultraviyole (UV) radyasyondan, yani güneş ışığından korumak için melanin üretir. Çoğu benler (Nevüs) iyi huyludur, ancak bazen bir iyi huylu görünen benlerde kötü huylu ve kontrolsüz melanosit hareketleri olabilir.
Melanomun nedeni nedir?
Melanom, melanositler olarak bilinen pigment üreten hücreler mutasyona uğradığında gelişir. Çoğu melanosit ciltte bulunmasına rağmen, bazıları gözlerde ve vücudun diğer kısımlarında görülür. Hastalığın kesin nedeni her zaman net olmasa da, birincil risk faktörü güneşten veya bronzlaşma yataklarından ultraviyole (UV) radyasyona maruz kalmaktır. Özellikle çocukken sık sık güneş yanığı olan kişilerin riski daha yüksektir.
Risk faktörleri
Risk faktörlerini anlamak, hastalığı geliştirme olasılığını azaltmak için önleyici tedbirler almanıza yardımcı olabilir. Bu faktörleri azaltmak, melanom veya diğer cilt kanserleri riskini azaltacaktır. Kontrol edilemeyen faktörler için, düzenli cilt muayeneleri erken tanı açısından çok önemlidir. Bu risk faktörleri şöyledir:
- Genel – Ultraviyoleye (UV) maruz kalma: Gün boyunca açık havada çalışan veya boş zamanlarının çoğunu açık havada geçirmeyi seçen ve UV ışığına maruz kalan insanlar daha fazla risk altındadır. Bronzlaşma yataklarını kullanmayı seçen insanlar cilt kanseri riskini artırır. Sık sık güneş yanığı, özellikle çocuklukta meydana geldiklerinde, hastalığın gelişme riskini arttırır.
- Yaş: Birçok kanserde olduğu gibi, yaşlandıkça melanom riskleri artar. Yeni vakalarının yaklaşık yarısı 55-74 yaş arası hastalarda teşhis edilir. Ancak bu hastalık her yaştan insanı etkileyebilir. Aslında, 25 ila 29 yaş arası kadınlar arasında en yaygın kanser türüdür.
- Bağışıklık baskılama: Organ nakli ile ilişkili virüsler, hastalıklar veya bağışıklık baskılama terapisi gibi bağışıklık sistemini zayıflatan koşullar tüm cilt kanserleri için riskleri artırabilir.
- Vücut – Cilt tonu: Kafkasyalıların cilt kanseri geliştirme riski beyaz olmayanlardan daha fazladır. Sarı veya kızıl saçlı, mavi veya yeşil gözlü veya kolayca yanabilen veya çilli cilde sahip kişiler için de risk daha yüksektir.
- Benler (Nevüs): Çoğu ben zararsızdır ve asla kansere dönüşmez, ancak çok sayıda benin olması melanom gelişme riskini artırabilir. Displastik nevus (melanomu andırabilecek benler) varlığı da riski yüzde 10 oranında artırabilir. Her ne kadar displastik nevuslar melanom haline gelmeyecek olsa da, küçük bir yüzde olabilir ve bu tip benlere sahip bireyler kapsamlı cilt muayeneleri için düzenli olarak bir dermatoloğa gitmelidir. (Dermatoloji, cilt hastalıkları ve tedavisiyle ilgilenen tıp dalı. İlgilenen hekimin adı Dermatologdur.)
- Genetik – Aile ve / veya kişisel geçmiş: Anne, baba ve kardeşlerde bu hastalık varsa risk artar. Daha önce hastalık tanısı konan bireyler de hastalığı tekrar geliştirme riski altındadır.
- Kalıtsal koşullar: Cildin UV hasarını onarma yeteneğini etkileyen kalıtsal bir hastalık olan Xeroderma Pigmentosum gibi durumlar, melanom geliştirme riski artar ve daha erken yaşta gelişebilir.
Melanom Türleri
En yaygın melanom tipi ciltte gelişen kutanöz türüdür. Çoğu melanom güneşe maruz kalan ciltte gelişirken, hastalık kasık veya ayakların dipleri gibi maruz kalmayan bölgelerde de bulunabilir.
Yüzeysel yayılan melanom

Yüzeysel yayılan melanom en sık görülen türdür (%70). Hastalığın bu formu, cildin dış tabakası boyunca birkaç yıl boyunca büyüyebilir. Yüzeysel yayılan melanomlar yükselebilir ve düzensiz sınırları olabilir. Siyah veya pembe kenarlı kahverengi olabilirler. Ulusal Kanser Enstitüsü’ne (NCI) göre, teşhis edilen vakaların yüzde yetmişi yüzeysel yayılan türdendir.
Nodüler melanom

Cildin yüzeyinde ilk kez ortaya çıktıktan sonra, nodüler melanom hızla cildin daha derin katmanlarına dönüşebilir. Hastalığın bu formu bir yumru veya büyüme olarak görünebilir. Nodüler melanomlar tüm vakaların yüzde 15’ini oluşturur.
Akral-lentiginöz melanom

Akral-lentiginöz melanom en koyu tenli kişilerde en yaygın olanıdır. NCI’ye göre, bu tip melanom Afrika kökenli Amerikalılarda hastalığın yüzde 70’ini ve Asyalılar’daki tüm vakaların yüzde 46’sını temsil ediyor. Akral-lentiginöz melanom, avuç içlerinde, ayak tabanlarında ve tırnakların altında bulunabilir.
Lentigo maligna melanomu

Lentingo maligna melanomları çoğunlukla kollarda, bacaklarda, yüzde, boyunda ve güneşe maruz kalan diğer bölgelerde bulunur. Bu tip melanom riski, uzun süre güneşe maruz kalması nedeniyle yaşla birlikte artabilir. Cilt Kanseri Vakfı’na göre, Lentingo maligna Hawaii’deki en yaygın türdür.
Amelanotik ve desmoplastik melanomlar

Bu iki benzer ve nadir melanom formu agresif olabilir ve teşhis edilmesi zor olabilir. Amelanotik melanomun pigment eksikliği nedeniyle tespit edilmesi zor olabilir. Desmoplastik melanom yaşlı hastaların baş ve boynunda bulunabilir.
Oküler melanom

Gözlere renk veren melanositlerde oküler melanom gelişir. Tüm vakaların yaklaşık yüzde 3’ünü oluşturmaktadır. Her yıl 2.000’den fazla vaka teşhis edilir.
Metastatik Melanom
Uzak organlara yayılan melanoma türüdür. Hastalık çoğunlukla akciğerlere, karaciğere, kemiğe ve / veya beyine yayılır.
Melanom belirtileri nelerdir?
Çoğu melanom cilt üzerinde gelişir ve erken tespit edilebilir. Kendi kendine muayene veya bir doktor tarafından yapılan düzenli cilt muayeneleri, şüpheli benleri veya deride erken belirtiler olabilecek değişiklikleri tespit etmeye yardımcı olabilir.
Diğer semptomlar şunları içerir:
- İyileşmeyen yaralar
- Kızarıklık, şişme veya hassas cilt
- Benlerde büyüme, şekilsizlik, renk değişikliği veya kanama
- Gözlerde koyu lekeler, görme kaybı veya bulanık görme
Melanomun erken uyarı işaretleri
İlk belirtisi tipik olarak ciltte yeni bir noktadır veya mevcut bir leke veya benin büyüklüğünde, şeklinde veya renginde bir değişikliktir.
- Asimetri: leke veya ben düzensiz bir şekle sahiptir.
- Kenarlık: Kenar pürüzsüz değil, düzensiz veya çentikli.
- Renk: ben düzensiz gölgeleme veya koyu lekelere sahiptir.
- Çap: Ben bir kalem silgisinin boyutundan daha büyüktür.
- Yükseklik: Ben boyut, şekil veya doku olarak değişiyor.
Melanom Evreleri
Melanom fizik muayene ve görüntüleme sonuçlarına göre ameliyattan önce (klinik evreleme) evrelendirilebilir. Ayrıca klinik bilginin biyopsilerden elde edilen bilgilerle birleştirileceği ameliyattan sonra (patolojik evreleme) evrelendirilecektir. Daha fazla bilgi kullandığı için patolojik kanser evrelemesi en doğrudur.
Melanom Evreleri:
- Evre 0: Kanser hücreleri cildin üst tabakasında (epidermis) ve yayılmamıştır. Bu aşamada, kanser genellikle sadece ameliyatla tedavi edilir.
- Evre I: Kanser hücreleri cildin derinliklerinde büyümüştür, ancak lenf düğümlerine veya vücudun diğer kısımlarına yayılmamıştır.
- Evre II: Kanser hücreleri cildin derinliklerine iner veya daha yüksek riskli özelliklere sahiptir, ancak lenf düğümlerine veya ötesine yayılmamıştır.
- Evre III: Kanser hücreleri yakındaki lenf düğümlerine yayılmış, ancak uzak organlara yayılmamıştır.
- Evre IV: Metastatik melanom olarak da bilinir, kanser hücrelerinin deri ve bölgesel lenf düğümlerinin ötesine geçerek karaciğer, akciğerler veya beyin gibi uzak organlara veya uzak lenf düğümleri ve bölgelerine yayıldığı anlamına gelir.
Teşhis
Melanom tanısı genellikle görsel bir muayene ile başlar. Aylık kendi kendine muayene ve yıllık doktor kontrolleri önemlidir.
Bir leke veya benin melanom olup olmadığından emin olmanın tek yolu, bir doktor tarafından muayene edilmesidir.
Melanom teşhisi için bazı testler:
Biyopsi
Lokal anestezi altında bölgeden parça alınarak patolojiye gönderilebilir. Deri kanserlerinin teşhisinde çeşitli biyopsi yöntemleri kullanılır, ancak şüpheli duurmlarda doktorlar genellikle tüm büyümenin çıkarıldığı eksizyonel biyopsi kullanmayı tercih ederler.
Melanom teşhisi konulursa, doktorunuz kanserin cildin ötesine yayılıp yayılmadığını belirlemek için bazı testler yapabilir. Genellikle yayılan ilk yer melanomlar yakındaki lenf düğümlerine aittir, bu nedenle doktorunuz herhangi bir lenf düğümünün genişleyip genişlemediğini belirlemek için koltuk altı, baş, boyun ve kasık bölgesini muayene edebilir. Doktor ayrıca şüpheli lenf düğümlerinin biyopsisini alabilir. İşlem sırasında cerrah bir sentinel lenf düğümü biyopsisi yapabilir.
Görüntüleme
Melanomun metastaz yapma veya uzak kemiklere veya uzak organlara yayılma diğer cilt kanserlerinden daha olasıdır. CT taraması, MRI, PET / CT taraması veya X-ışını dahil olmak üzere çeşitli tıbbi görüntüleme prosedürleri, vücuttaki kanser hücrelerini veya tümörleri tespit etmek için kullanılabilir.
Melanom tedavileri
Melanom tedavisi, tek başına veya kombinasyon halinde cerrahi, radyasyon terapisi, kemoterapi, immünoterapi veya hedefli tedaviyi içerebilir. Tedavi planınız genellikle hastalığın ne kadar erken teşhis edildiğine ve yayılıp yayılmadığına bağlıdır.
Kemoterapi
Vücudun uzak bölgelerine yayılmış (metastatik) hastalar için kemoterapi önerilebilir. Kemoterapi, immünoterapi ve cerrahi dahil olmak üzere diğer kanser tedavileri ile kombinasyon halinde kullanılabilir.

Bacak veya kol gibi ekstremitelerin birinde tümör bulunduğunda uzuvdan etkilenen bazı melanom vakalarında bölgesel kemoterapi veya izole ekstremite infüzyonu önerilebilir. Bu durumlarda, izole ekstremite infüzyonu, tümörü tedavi etmek ve kemoterapinin vücudun başka bir yerine gitmesini önlemeye yardımcı olmak için kemoterapiyi doğrudan etkilenen uzuvya uygular. Kemoterapiyi etkilenen bölgeye konsantre ederek, bu teknik sistemik kemoterapiden daha az yan etkiye neden olabilir. Bu prosedürde, kol veya bacağa bir turnike yerleştirilir, daha sonra yüksek dozlarda kemoterapi uygulanır.
İmmünoterapi
İmmünoterapi ilaçları, melanom ve diğer bazı kanserler için birinci basamak tedavi olarak kullanılabilir veya kemoterapi ve cerrahi gibi diğer tedavilerle kombinasyon halinde kullanılabilir. Örneğin: Kontrol noktası inhibitörleri, Sitokinler, Onkolitik virüs tedavisi.
Radyasyon tedavisi
Radyasyon tedavisi ileri hastalık için kullanılabilir. Kullanılan spesifik tedaviler şunları içerir:
Dış ışın radyasyon tedavisi, cerrahi ile ilişkili standart risklerin veya komplikasyonların hiçbirini taşımayan ve size veya temas ettiğiniz diğer kişilere radyoaktivite riski taşımayan ağrısız bir ayakta tedavi prosedürüdür.
Yoğunluk ayarlı radyasyon tedavisi, hastaların rekürrens riskini azaltmasına ve tedavileri daha hızlı bitirmesine yardımcı olabilir.
TomoTherapy® ulaşılması zor melanom tümörlerini hedefler ve yakındaki sağlıklı dokuya verilen zararı azaltmaya yardımcı olarak tedaviyle ilgili yan etkileri azaltır.
Ameliyat
Cerrahi lokalize melanom için birincil tedavidir. Metastaz yapmış hastalık için bir tedavi seçeneği olabilir. Bazı lokalize melanomlar için gerekli olan tek tedavi cerrahi olabilir. Bununla birlikte, yakınlardaki lenf düğümleri büyürse ve doktor kanser hücrelerinin yayıldığından şüphelenirse daha kapsamlı ameliyatlar gerektirebilir.
Melanom için cerrahi prosedürler şunları içerir:
Eksizyon: Cerrah, lokal anestezi altında neşter ile bir eksizyon uygulayarak cildin büyümesini keser. Melanomlarda tipik olarak geniş bir eksizyon kullanılır. Geniş bir eksizyonda, deri tümörü ve daha geniş bir sağlıklı doku çevresi çıkarılır. Geniş bir eksizyon, basit bir eksizyondan çok daha derin bir deriye uzanabilir (bkz. Eksizyonel Biyopsi)
Rekonstrüktif cerrahi: Cilt kanseri ameliyatları, özellikle cilt kanserini çıkarmak için geniş bir eksizyon veya başka bir kapsamlı ameliyat gerektiğinde veya ameliyat yüz, baş, boyun veya ellerde yapıldığında yara izi veya şekil bozukluğuna neden olabilir. Rekonstrüktif cerrahi seçenekleriniz hakkında doktorunuza danışın.
Lenf nodu biyopsisi ve çıkarılması: Bu prosedürde, doktorunuz doğrudan tümörden drene olan lenf sıvısını alan sentinel lenf düğümleri olarak bilinen bir veya daha fazla lenf düğümünü çıkaracaktır. Lenf düğümü veya düğümlerinde kanser belirtisi yoksa, ilave lenf düğümü ameliyatı gerekmez. Melanom hücreleri bir veya daha fazla sentinel lenf nodunda bulunursa, bölgedeki kalan lenf nodları çıkarılabilir.
Sentinel lenf nodu biyopsisi: Melanomlu hastalarda, sentinel lenf nodu olarak bilinen özel tipte bir lenf nodu biyopsisi sıklıkla yapılır. Bu prosedürde, doktorunuz sentinel lenf düğümleri olarak bilinen ve tümörden drenaj yapan lenf sıvısını alması muhtemel bir veya birkaç spesifik lenf düğümünü çıkaracaktır. Sentinel lenf nodu kanser belirtisi göstermezse, ek lenf nodu ameliyatı gerekmez. Melanom hücreleri bir veya daha fazla sentinel lenf nodunda bulunursa, bölgedeki kalan lenf nodları genellikle çıkarılır. Sentinel lenf nodu biyopsisi, geleneksel lenf nodu diseksiyonundan daha az invaziv bir prosedürdür ve tipik olarak lenfödem gibi daha az yan etki ile ilişkilidir.
Metastatik melanom için cerrahi: Melanom beyne, kemiklere, karaciğere ve akciğerlere yayılabilir. Bu meydana geldiğinde, tümörlerin bu konumlardan çıkarılması için ameliyat yapılabilir. Tedavide cerrahi, immünoterapi veya kemoterapi gibi diğer tedavilerle birleştirilebilir. Bazı durumlarda, hastalığın semptomlarını hafifletmek için metastatik melanom cerrahisi önerilebilir (Palyatif Cerrahi)
Hedefli terapi
FDA, cerrahi ile çıkarılamayan ileri metastatik melanomu tedavi etmek için birkaç hedefe yönelik tedavi ilacını onaylamıştır. Bazı hedefe yönelik tedavi ilaçları, cerrahi ile tedavi edilemeyen durumlarda kullanılır.