Kolorektal kanser genellikle kolon veya rektum içindeki polip adı verilen bir büyüme olarak başlar. Poliplerin bulunması ve çıkarılması kolorektal kanseri önleyebilir. Kolorektal kanserle ilgili önleme, tarama, tedavi, istatistik, araştırma, klinik deneyler ve daha fazlası hakkında daha fazla bilgi edinmek için bu makaleyi ele aldım.
Kolon kanseri nedir?
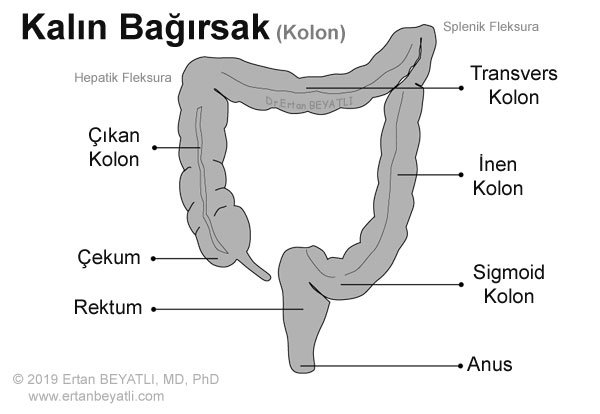
Kolon kanseri (genellikle kolorektal kanser olarak adlandırılır) erken aşamalarda tespit edilirse önlenebilir ve yüksek oranda tedavi edilebilir. Kısaltması Kolon CA. İngilizcesi “Colon Cancer” dir. Kolon, kalın bağırsağın en uzun kısmıdır. Çekumdan sindirilmiş yiyecekleri alır, su ve besinleri emer ve atıkları (dışkı) rektuma geçirir. Kolon 4 bölüme ayrılmıştır.
- Çıkan kolon (assendan), kolonun başlangıcıdır ve karnın sağ tarafında bulunur. Karaciğerde bükülme denilen (Hepatik fleksura) kolondaki bir kıvrıma kadar devam eder.
- Transvers kolon, çıkan kolonu ve hepatik fleksurayı takip eder. Karnın üst kısmı boyunca uzanır. Dalak bükülmesi (Splenik fleksura) denilen kolonda bir kıvrım ile sonlanır.
- İnen kolon (Dessendan), transvers kolon ve splenik fleksurayı takip eder. Karnın sol tarafında bulunur.
- Sigmoid kolon, kolonun rektuma bağlanan son kısmıdır.
Kolorektal kanser İngiltere’de ikinci, Amerika’da üçüncü ölüm nedenidir. Kolorektal kanser, sıklık açısından dünyada kadınlarda 2. ve erkeklerde 3. en sık görülen kanserdir. Bunun yüzde 70’lik kısmını kolon kanseri, geri kalan kısmını ise rektum kanseri oluşturur. Kolorektal kanserin özellikle ailevi olmayan tipinde yaş önemli bir risk faktörüdür. 40 yaşından itibaren risk artmaktadır. Özellikle ABD’de kolorektal kansere yakalanma oranı yüzde 5’tir ve kolorektal kanser tanılı hastaların yüzde 90’ı 50 yaş üzerindedir.
Erkeklerde görülme sıklığı kadınlara göre yüzde 25 daha fazladır. Son zamanlarda sağ taraf kolon kanserleri sol tarafa göre daha çok görülmektedir. Kolonoskopi yapılma oranının 1980’den beri artması bu kanserlerin erken yakalanma şansını arttırmış ve yeni etkili tedavi yöntemleriyle de hastaların sağ kalım süreleri uzamıştır.
RİSK FAKTÖRLERİ
Kolorektal kanserin kesin nedeni bilinmemektedir. Bununla birlikte, bazı genetik nedenlerin anlaşılması artmaya devam etmektedir. Aşağıdaki faktörler kişinin kolorektal kanser riskini artırabilir:
- Yaş: İnsanların %90’ından fazlasına 50 yaşından sonra kolorektal kanser tanısı konmaktadır.
- Kolorektal kanserin aile öyküsü (özellikle ebeveynler veya kardeşler).
- Sekiz yıl veya daha uzun süre kişisel Crohn hastalığı veya ülseratif kolit öyküsü (İBH).
- Kolorektal polipler.
- Kişisel meme, uterin veya yumurtalık kanseri öyküsü.
- Şeker hastalığı. Tip 2 Diyabet hastalarının kolorektal kanser geliştirme olasılığı diğer insanlardan daha fazladır.
- Diyet. Çok fazla yağ, kolesterol ve az miktarda lif yiyenlerin kolorektal kanser geliştirme olasılığı daha yüksektir.
- Yaşam tarzı. Çok miktarda alkol tüketirseniz, sigara içiyorsanız, egzersiz yapmıyorsanız ve fazla kiloluysanız (Obezite), kolorektal kansere yakalanma olasılığınız daha yüksek olabilir.
Kolon kanseri riskini artıran kalıtsal gen mutasyonları
Kolon kanseri riskini artıran kalıtsal gen mutasyonları ailelerden geçebilir, ancak bu kalıtsal genler sadece küçük (5%) bir kolon kanseri yüzdesiyle bağlantılıdır. Kalıtsal gen mutasyonları kanseri kaçınılmaz kılmaz, ancak bir bireyin kanser riskini önemli ölçüde artırabilir.
Kalıtsal kolon kanseri sendromlarının en sık görülen formları:
- Kalıtsal Polipsiz-olmayan kolorektal kanser (HNPCC). Lynch sendromu olarak da adlandırılan HNPCC, kolon kanseri ve diğer kanser riskini arttırır. HNPCC’li insanlar 50 yaşından önce kolon kanseri geliştirme eğilimindedir.
- Ailesel adenomatoz polipozis (FAP). FAP, kolon ve rektumun astarında binlerce polip geliştirmenize neden olan nadir bir hastalıktır. Tedavi edilmemiş FAP’lı insanlar, 40 yaşından önce kolon kanseri gelişme riskini büyük ölçüde artırır.
Diyet ve kolon kanseri arasındaki ilişki
Yapılan klinik çalışmalar, tipik bir Batılı diyet ile artmış kolon kanseri riski arasında bir ilişki olduğunu göstermiştir. Tipik bir Batı diyeti, yağ bakımından yüksek ve lif bakımından düşüktür. İnsanlar, tipik diyetin yağ oranı düşük ve lif bakımından yüksek olduğu bölgelerden tipik Batı diyetinin en yaygın olduğu alanlara geçtiğinde, bu kişilerde kolon kanseri riski önemli ölçüde artar. Bu durumun nedeni henüz belli değil, ancak araştırmacılar, yüksek yağlı, düşük lifli bir diyetin kolonda yaşayan mikropları etkileyip etkilemediğini veya kanser riskine katkıda bulunabilecek altta yatan iltihaplanmaya neden olup olmadığını inceliyorlar. Bu aktif bir araştırma alanıdır ve araştırmalar devam etmektedir.
ÖNLEME
Neredeyse tüm kolorektal kanser vakaları poliplerden ortaya çıkar. Kolonun iç astarından başlarlar ve en sık kolonun sol tarafını etkilerler. Poliplerin kolonoskopi ile tespiti ve çıkarılması (Kolonoskopik Polipektomi – Youtube video izle) kolorektal kanser riskini azaltır. Kolorektal kanser tarama önerileri tıbbi ve aile öyküsüne dayanmaktadır. Tarama tipik olarak ortalama risk taşıyan hastalarda 45 yaşında başlar. Daha yüksek risk altındakilere genellikle ilk taramalarını genç yaşta almaları önerilir.
Kesin olmamakla birlikte, kolorektal kanseri önlemede diyetin önemli bir rol oynayabileceğine dair bazı kanıtlar vardır. Lif bakımından yüksek (tam tahıllar, meyveler, sebzeler ve kuruyemişler) ve yağ oranı düşük diyet kolorektal kanseri önlemeye yardımcı olabilecek tek diyet önlemidir. 2018 yılında, 50 yaşın altındaki hastalarda kolon kanseri riskindeki artışa ilişkin yeni verilere ikincil olarak, Amerikan Kolon ve Rektum Cerrahisi Derneği, 45 yaşında taramayı başlatmak için önerileri değiştirdi.
Belirtiler
Kolorektal kanser sıklıkla belirti vermez ve rutin taramalar sırasında tespit edilir. Diğer yaygın sağlık sorunlarının aynı semptomların bazılarına neden olabileceğini not etmek önemlidir. Örneğin, hemoroidler rektal kanamanın yaygın bir nedenidir, ancak kolorektal kansere neden olmaz. Kolorektal kanser belirtileri şunlardır:
- Bağırsak alışkanlıklarında değişiklik (kabızlık veya ishal).
- Dar şekilli dışkılama.
- Dışkıda parlak kırmızı ya da çok koyu kan.
- Devam eden pelvik veya alt karın ağrısı (örneğin, gaz, şişkinlik veya ağrı).
- Açıklanamayan kilo kaybı.
- Mide bulantısı ya da kusma.
- Sürekli yorgunluk hissi.
Karın ağrısı ve kilo kaybı tipik olarak geç semptomlardır ve bu da geniş kapsamlı bir hastalığa işaret eder. Yukarıdaki semptomlardan herhangi birini yaşayan herkes en kısa zamanda bir doktora görünmelidir.
Dr. Ertan Beyatlı
Kolon CA Tanısı
- Fiziki muayene ve tıbbi özgeçmiş.
- Kan testleri
- Gaitada Gizli Kan (GGK) testi
- Kolonoskopi: Tüm kolonun kameralı, uzun ve ince, esnek bir tüple ve ucunda bir ışıkla incelenmesi (kolonoskop).
- Biyopsi: Hücrelerin veya dokuların çıkarılması kanser belirtilerini kontrol etmek için mikroskop altında görülebilir.
Evreleme için aşağıdaki testler kullanılabilir:
- CEA tahlili: Karsinoembriyonik antijen, kanser varsa kanda yükselebilecek bir maddedir. Tamamen kendi başına kesin olmasa da, bu test genellikle diğer tanı testleriyle yapılır.
- Abdominal ultrason: Karaciğer, safra kesesi, pankreas veya karın içindeki herhangi bir yere yayılmış tümörleri gösterir.
- Bilgisayarlı Tomografi (BT) taraması: Kolon dışına yayılmış olan çoğu kanser hücresinin varlığını doğru bir şekilde tespit edebilir.
- Manyetik Rezonans imagin (MRI): Tümörün rektumun duvarı boyunca yayılıp yayılmadığını ve yakındaki yapıları işgal edip etmediğini (invazyon) belirlemeye yardımcı olur.
- Pozitron emisyon tomografi (PET) taraması: Radyoaktif izleri olan özel bir boya kullanan bir görüntüleme testi. Bu, doktorların kolon dışına yayılmış olan (metastaz) çoğu kanser hücresinin varlığını tespit etmesini sağlar.
Kolorektal Kanser Sınıflaması (Staging)
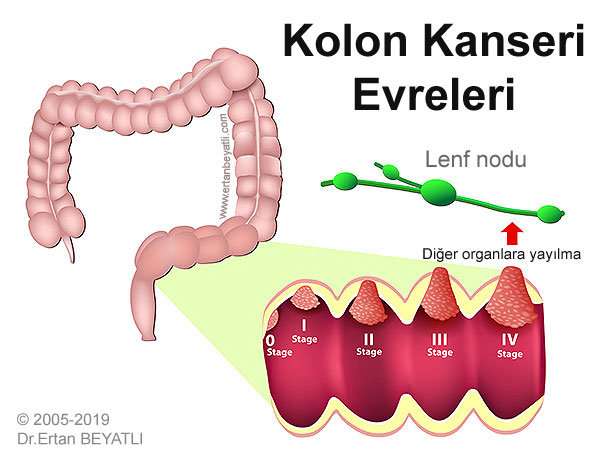
Kanserin kapsamı (klinik evre) tedavi kararını verme ve tedavi sonrası hasta sonucu ile bağlantılıdır. Evreleme, tümörün yakındaki dokuları mı, lenf nodlarını mı işgal ettiğine ve / veya kanserin vücudun diğer kısımlarına yayılmış olup (metastaz) olmamasına dayanır. Kesin evre genellikle ameliyattan sonraya kadar belli değildir.
- Stage 0: En erken aşamadır. Kanser başladığı yerden hareket etmedi; hala kolonun en iç astarı ile sınırlıdır. Bu aşamaya “Carcinoma in Situ” da denir.
- Stage I: Kanser yayılmaya başladı, ancak hala iç astarda. Aşama I ayrıca Dukes A kolon kanseri olarak da adlandırılır.
- Stage II: Kanserlerin çoğu kolonun duvarı boyunca büyümüş ve yakındaki dokulara uzanabilmiştir. Henüz lenf bezlerine yayılmadılar. Aşama II ayrıca Dukes B kolon kanseri olarak da adlandırılır.
- Stage III: Kanser lenf düğümlerine yayılmış, ancak vücudun uzak bölgelerine taşınmamıştır. Evre III ayrıca Dukes C kolon kanseri olarak da adlandırılır.
- Stage IV: Kanser lenf sistemi boyunca vücudun uzak bölgelerine, en sık akciğer ve karaciğere taşınmıştır. Bu “METASTAZ” olarak bilinir. Evre IV ayrıca Dukes D kolon kanseri olarak da adlandırılır.
TNM Evrelemesi
Tümör (T): tümörün boyutunu (kanser alanı) tarif eder. Bu, T aşamasının basitleştirilmiş bir açıklamasıdır. Bağırsak kanserinde 4 evre tümör evresi vardır:
- T1, tümörün sadece bağırsak iç katmanında olduğu anlamına gelir
- T2, tümörün bağırsak duvarının kas katmanına büyüdüğü anlamına gelir
- T3, tümörün bağırsak duvarının dış astarına doğru büyüdüğü anlamına gelir
- T4, tümörün bağırsak duvarının dış astarından (bağırsakların başka bir kısmına, yakındaki bir organ veya yapının içine) büyüdüğü anlamına gelir.

Düğüm (N): kanserin lenf düğümlerine yayılıp yayılmadığını açıklar. Kanser hücrelerinin lenf düğümlerinde olup olmadığını açıklayan 3 olası aşama vardır:
- N0, kanser hücrelerini içeren hiçbir lenf düğümü yoktur
- N1, bağırsaklara yakın 1-3 lenf nodu kanser hücreleri içeriyor
- N2, 4 veya daha fazla yakındaki lenf nodunda kanser hücresi mevcut
Metastaz (M): kanserin vücudun farklı bir bölgesine yayılmış olup olmadığını açıklar. 2 kanser yayılım evresi vardır (metastaz):
- M0, kanserin diğer organlara yayılmadığı anlamına gelir
- M1, kanserin vücudun diğer bölgelerine yayıldığı anlamına gelir

CERRAHİ TEDAVİ
Kolorektal kanseri için ameliyat neredeyse her zaman gereklidir. Tümör ve lenf düğümleri, tümörün her iki tarafında küçük bir kısım normal kolonla birlikte çıkarılır. Bu ameliyatların genel adı Kolektomi’dir.
Kolektomi nedir?
Kolektomi, kolonun tamamı veya bir kısmını çıkarmak için yapılan bir ameliyattır. Kolonu etkileyen hastalıkların tedavisinde uygulanır. Kolektomi ameliyatında genellikle sindirim sisteminizin kalan kısımlarını yeniden birleştirilmesi veya karın duvarına dikilmesi gerekir. Kolektominin 4 ana çeşidi vardır:
- Total kolektomi, tüm kolonun çıkarılmasını içerir.
- Parsiyel kolektomi, kolonun bir kısmının çıkarılmasını içerir ve subtotal kolektomi olarak da adlandırılır.
- Hemikolektomi, kolonun sağ veya sol kısmının çıkarılmasını içerir.
- Proktokolektomi, hem kolonun hem de rektumun çıkarılmasını içerir. Bu ameliyata İleostomi eklenir.
Kolostomi, kolonun bir kısmını karın duvarının cildine bağlayan, cerrahi olarak oluşturulmuş bir açıklıktır. Bu prosedür tipik olarak sadece çok az sayıda kolorektal kanser hastasında yapılır.
Minimal invaziv cerrahi teknikler, bireysel vakalara dayanarak eğitimli cerrahlar tarafından kullanılabilir. Cerrahınız ameliyat öncesi sizinle görüşecek ve en uygun yaklaşıma karar verecektir.
TIBBİ TEDAVİ
Kemoterapi, kanserin evresine bağlı olarak, ameliyattan önce ve / veya sonra uygulanabilir. Rektal kanserin aksine, radyasyon tedavisi kolorektal kanser için nadiren kullanılır.
PROGNOZ
Hasta sonuçları, tanı anında kolorektal kanser evresi ile güçlü bir şekilde ilişkilidir. Kolonun astarıyla sınırlı olan kanser, en yüksek başarı olasılığıyla ilişkilidir. Bu, kolonoskopi gibi tarama yöntemleriyle erken saptanmanın çok önemli olmasının bir nedenidir.
Kolorektal kanser için tedavi sonrası takip ve kontrol önemlidir. Kanser tamamen çıkarılmış veya tahrip olmuş gibi görünse bile, hastalık tekrarlayabilir. Belirlenmemiş kanser hücreleri tedaviden sonra vücutta kalabilir. Kolon ve rektum cerrahınız iyileşmenizi izler ve belirli aralıklarla kanser tekrarını kontrol eder. Kanserin evresine göre kan testleri, klinik muayeneler ve görüntüleme testleri yapılabilir.
KOLOREKTAL CERRAHİ NEDİR?
Kolon ve rektum cerrahları (Kolorektal cerrahi), kolon, rektum ve anüs hastalıklarının cerrahi ve cerrahi olmayan tedavisinde uzmandır.
Hazırlayan, Derleyen ve çeviren: Ertan BEYATLI, MD, PhD
Kaynaklar:
https://www.ccalliance.org/colorectal-cancer-information/stage-of-diagnosis
https://www.fascrs.org/patients/disease-condition/colon-cancer
http://www.cancer.ca/en/cancer-information/cancer-type/colorectal/colorectal-cancer/the-colon-and-rectum/?region=on
https://www.mayoclinic.org/diseases-conditions/colon-cancer/symptoms-causes/syc-20353669
https://www.webmd.com/colorectal-cancer/guide/staging-colon-rectal-cancer#1
https://www.cancerresearchuk.org/about-cancer/bowel-cancer/stages-types-and-grades/TNM-staging