ADBG – Ayakta Direk Batın Grafisi (Düz Karın Grafisi)
- ADBG filmi dik durarak ayakta çekilen karın grafisidir.
- Acil durumlarda çekilir. Örneğin:
- böbrek sancısı (Renal Kolik),
- Barsak Tıkanması (İleus, Sub-ileus, Volvulus),
- Barsak ve Mide Delinmesi (perforasyon),
- Apandisit, intesusepsiyon,
- Yabancı Cisim yutulması veya makattan sokulması
- Çekim sonrası, ADBG yorumlanması çok önemlidir. Özellikle travmaya bağlı hava sıvı seviyesinin tespiti, bağırsak tıkanmaları, gazların ve yumuşak dokudaki anormal yapıların gözlemlenmesi amacı ile çekilir.
- Latince’de standing direct abdominal radiograph olarak yazılır.


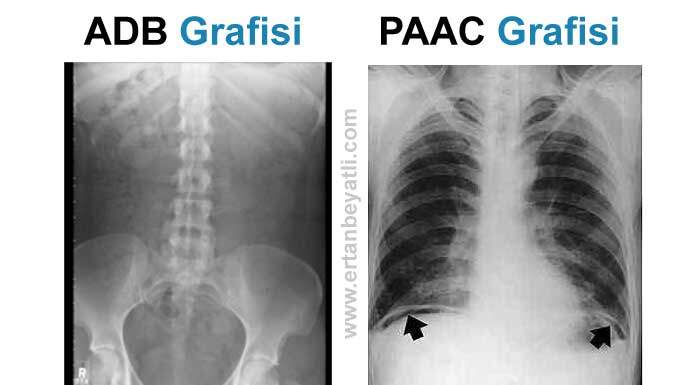
Diyafragm altında görülen serbest hava (subdiyafragmatik ters hilal bulgusu) PA Akciğer Grafisinde daha net bir şekilde görülür.
ADBG Nasıl çekilir?
Gebelerde sakıncalıdır ve çekilmez. Hastaya tek kullanımlık önlük verilerek kıyafetlerini ve varsa kolyesini çıkarıp verilen önlüğü giymesi istenir.
Çekim ayakta ve P-A (Arka-Ön) pozisyonunda yapılmalıdır.Hastanın karnı statife değmelidir. Diyafram kubbelerinide kesmeyecek ölçüde kaset (35X43) veya dedektör seçimi yapılmalıdır. Tüp kaset mesafesi 100 cm olmalıdır. Santralizasyon iliak kanadın 5 cm üzerine filme dik olacak şekilde yapılmalıdır. Hasta pozisyonu ayarlanıp gerekli ölçülerde kolimasyon yapıldıktan sonra hastaya derin bir nefes alıp tutması (inspiryum) söylenir. Ortalama bir erişkin için 100 KV ve otomatik MaS ile çekim yapılabilir.
Dikkat edilmesi gerekenler
Hastaların bir çoğu iç çamaşır takı vs çıkarmayı unutmaktadır. Hasta çekim için hazırlandığında tekrar kontrol edilmelidir. Özellikle nefes tutturulan çekimlerde bir çok hasta verilen nefes komutunu yerine getiremez bunun önüne gecmek ve optimum görüntüyü elde edebilmek adına nefes komutu verildiğinde hasta gözlemlenerek nefes alıp tuttuğu kontrol edilmelidir. Özetlersek
- Hamilelik kimlik bilgileri ve şikayetini sorgula
- Mesafe 100 cm
- KV:110 MaS otomatik
- Derin inspiryum
PAAC (PosteroAnterior Akciğer Grafisi)
PA akciğer grafisi göğüs bölgesi için en sık çekilen filmdir. Açılımı PA posteroanterior arka-ön demektir. Kısaltılmışı PA ACG dir. İngilizcesi PACXR (PA Chest X-ray)
Hasta ayakta durarak göğsünü kasete yaslar ve 180 cm mesafeden arkadan X-ışınını ile film çekilir. Kalp ve ana damarlar kasetten uzak olduğu için normalden daha büyük görülür. PA akciğer grafisi hasta tam nefes aldığında (inspirasyon) çekilir. Verilen X-ray ışın miktarı filmin koyuluğunu belirler. Ayrıca filmlerin üzerinde yönler belirlenir. (R-Right-sağ, L-Left-Sol)
PA ACG Yorumlanması
Bu film aracılığıyla nefes borusu (trakea), göğüs ve kalp oranı (kardiyotorasik oran), şah damar (aort), akciğer, göğüs boşluğu (mediasten) ve diafragm değerlendirilir. Diyafragm altındaki serbest hava (sub-diafragmatik) Ayakta Direkt Batın Grafisinden (ADBG) daha net bir şekilde görülür. Örneğin Bağısak ve mide delinmeleri, apandisit patlaması durumları.

PA Akciğer Grafisi Ne zaman çekilir?
PA ACG akut ve kronik hastalıkların teşhis ve takibinde sıklıkla kullanılır. İşe giriş öncesinde sağlık kontrolü için çekilir. Ameliyat öncesi rutin tarama amacıyla çekilebilir. Öksürük, ateş veya ağrı gibi durumlarda çekilebilir. Ayrıca PA ACG zatüre (pnömoni), pulmoner ödem, KOAH veya plevral efüzyon açısından değerlendirilen mükemmel bir ilk görüntüleme testidir.
PA Akciğer Grafisi İşaretleri
Silüet işareti
Felson tarafından isimlendirilen bu işaret parankimal bir opasitenin anatomik olarak ilişkili olduğu yumuşak doku ile arasındaki sınırın silinmesine neden olacağını tanımlar. En sık kullanıldığı yumuşak doku kalp ve onun komşuluğundaki sağ orta lob ve lingulaya ait parankimdir. Bu alanlara ait havalanma kayıplarında aradaki sınır silineceğinden ve farklı alanlara ait patolojilerde aynı nedenlerden dolayı silinmeyeceğinden lezyon lokalizasyonu yapılabilir.
“Hilum overlay” işareti
Silüet işaretinin hiluslara uyarlanmış şeklidir. Hiler damarların lezyondan ayırt edilebildiği durumlarda lezyonun hilusun anterior ya da posteriorunda olduğu anlaşılır. Damarların lezyona bağlı silinmiş olması lezyon lokalizasyonunun hilus olduğunu gösterir. Hava bronkogramı Hava ile dolu bronşların hava içermeyen akciğer parankimi ile birlikte görünmesine verilen isimdir. Bu görünüm proksimal havayollarının açık olduğunu ve alveollerdeki havanın rezorbe olduğunu ya da replase edildiğine işaret eder. Rezorbsiyon nedeni atelektazi, replasman nedeni ise en sık pnömoni ya da pulmoner ödemdir.
Hilal bulgusu
Bir diğer adı menisküs işareti olan bu bulgu parankimal bir kavitenin duvarı ile içindeki kitle arasında hilal şeklinde hava birikmesidir. Tipik olarak kaviteler içerisinde Aspergillus kolonizasyonunda görülür. Bir diğer oluşma şekli anjioinvaziv aspergillloz olgularının iyileşme döneminde nekrotik parankimin retrakte olmasıdır.
Golden S bulgusu
Golden tarafından tanımlanan bu bulgu santral bir kitleye eşlik eden sağ üst lob atelektazisinde görülür. Minör fissürün medial kesimi inferiora konveks görünümdeyken, lateral kesimi inferiora konkav olarak izlenir. Bu değişiklikler PA grafide fissürün ters S şeklinde görülmesine neden olur. Servikotorasik işareti Toraks giriminde bulunan bir lezyonun mediastendeki lokalizasyonunu belirlemede yardımcıdır. Akciğer apeks parankimi posteriorda daha superior uzanıma sahip olduğundan, posterior mediasten yerleşimli bir lezyon PA grafide klavikulanun üzerine uzanır ve sınırları net seçilir. Anterior mediasten yerleşimli lezyonlar ise klavikulanın altında izlenir ve servikal yumuşak dokulardan ayırt edilemez.
Luftsichel işareti
Almanca hava ve orak kelimelerinin birleşmesinden oluşan bu işaret sol üst lob kollapsında görülür. Alt lob superior segmentin superiora deplase olarak arkus aorta ve atelektatik sol üst lob arasına girmesi sonucunda hiperlusan orak şeklinde bir görünüm oluşur.
Pala işareti
Kalbin sağ konturu boyunca diafragmaya uzanan anormal pulmoner vene ait kıvrımlı tubuler yapıya ait görünümdür. Anormal sağ inferior pulmoner ven genellikle hemidiafragma komşuluğunda inferior vena cavaya dökülür.
Hampton hörgücü bulgusu
Pulmoner infarkta sekonder gelişen ve geniş tabanıyla plevraya oturan bir opasitedir. Akciğer parankiminin bronşial arterlerden de beslenmesi nedeniyle lezyonun apeksi konveks görünümdedir. Opasifikasyonun nedeni ise pulmoner infarkta sekonder gelişen alveoler hemorajidir. Genellikle alt loblarda görülür ve lineer skar oluşumuyla düzelir.
Westermark bulgusu
Pulmoner embolide meydana gelen vazokonstriksiyona bağlı gelişen oligeminin neden olduğu azalmış periferik vaskülarizasyona işaret eder. PA grafilerde radyolusan alan olarak izlenir. Sensitivitesi düşük olmakla birlikte Hampton hörgücü bulgusu gibi yüksek spesifisiteye sahiptir.
Juxtaphrenic tepe işareti
Üst lob atelektazisi veya lobektomisinde aynı taraftaki diafragmanın orta kesiminde tepesi yukarıda bulunan üçgen şekilli opasite izlenmesine verilen isimdir. Atelektazide oluşan negatif basınca bağlı viseral plevranın superiora retraksiyonu ve bu hastalarda bulunan inferior aksesuar fissüre ekstraplevral yağ dokusunun protrzyonu sonucu geliştiği düşünülmektedir. Sağ akciğerde sola oranla daha sık görülür, sağ orta lob atelektazisinde de izlenebilir.